|
 |
- Search
| J Neurointensive Care > Volume 6(1); 2023 > Article |
|
This article has been corrected. See J Neurointensive Care. 2023 Oct 30; 6(2): 163.
Abstract
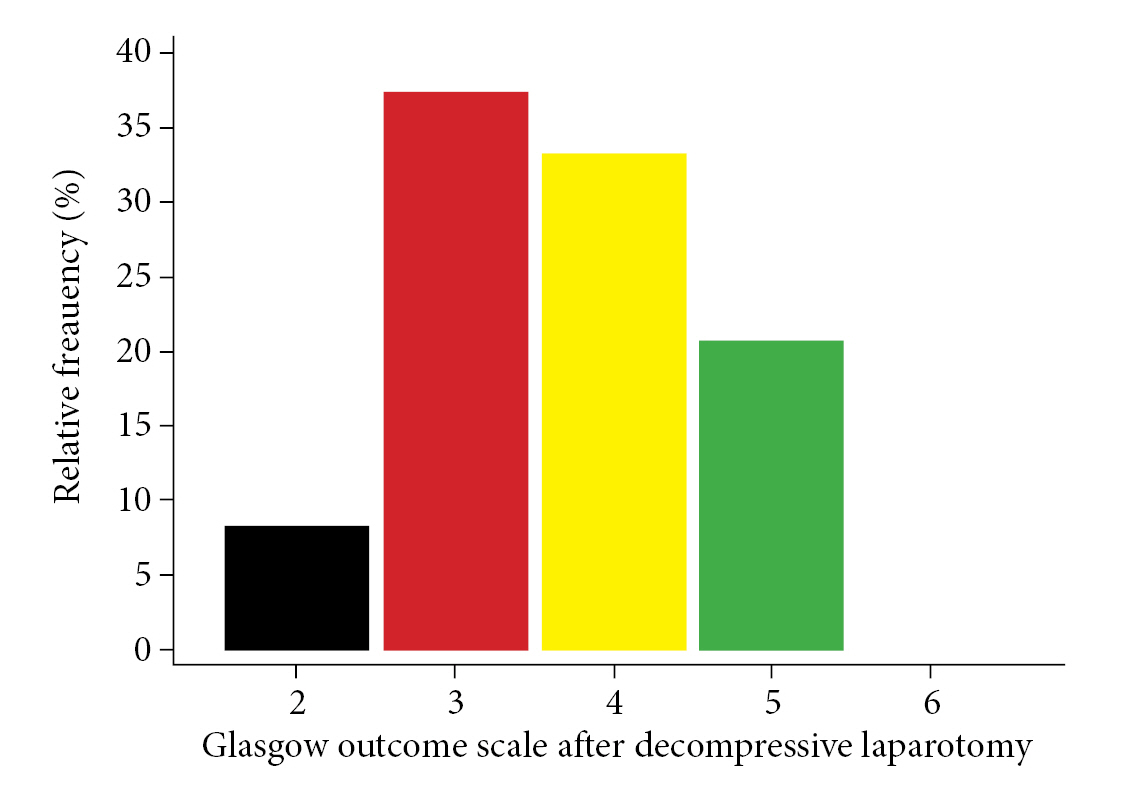
Researchers investigated the role of decompressive laparotomy as a novel technique to improve the outcome of refractory intracranial hypertension in patients with severe Traumatic brain injury (TBI). In this paper, we conduct a systematic review of the literature and discuss the existing information on the role of decompressive laparotomy in patients with severe TBI. A search for randomized controlled trial (RCT), not RCT, prospective and retrospective cohort studies will be carried out through electronic databases. The strategy comprised topic headings (MeSH) such as "Decompressive laparotomy," "traumatic brain damage," "Neurocritical care," and "intracranial hypertension," as well as text words related to Booleans terms. The following data were retrieved individually and separately: mortality, functional independence (modified Rankin scale 0 to 2, or Glasgow Prognostic Scale with a score of 4 or above), and intracranial pressure value before and after Decompressive laparotomy. Following a thorough text review, ten articles were examined for confidentiality, one of which is a narrative review, two of which did not cover traumatic brain injury and one of which included thoracic and neck trauma, and six of which were included for qualitative and quantitative analysis. Among the six trials considered, 46 patients with TBI and intracranial hypertension were evaluated and treated with hyperosmolar treatment and/or Decompressive Craniectomy with Decompressive laparotomy. The Glasgow Outcome Scale was used to evaluate neurological prognosis and functional competence.According to the findings, 8% of the patients were in a chronic vegetative state, 37.93% had severe disability, 33.45% had moderate disability, and the majority (64.3%) were able to return to work with limitations. The remaining 20.6% had mild disability or good functional recovery.
Elevated intracranial pressure has been associated with increased morbidity and mortality following a head injury1-3). The "staircase" management technique is the normal course of treatment for traumatic brain injury (TBI) patients with raised intracranial pressure; the higher the tier of drugs, the greater the risk of adverse effects and the narrower the benefit-to-risk ratio1,2). Decompressive craniectomy was used to reduce intracranial pressure in some patients with severe traumatic brain injury who were not candidates for conservative treatment4-6). In addition to these commonly used treatments, few studies have looked at the effect of several alternative life-saving therapies with different outcomes7,8). Decompressive laparotomy is one such treatment, and the researchers evaluated its role in improving the outcome of refractory intracranial hypertension in patients with severe TBI9-14). In this study, we conducted a systematic review of the literature and addressed the existing data on the role of decompressive laparotomy in patients with severe traumatic brain injury.
The investigation was carried out in compliance with the recommendations of the MOOSE declaration15) for the presentation of systematic reviews of observational studies, meta-analyses, and the Cochrane manual of systematic reviews and meta-analysis16). A search for randomized controlled trial (RCT), not RCT, prospective and retrospective cohort studies will be carried out through PUBMED (until May 2022); SCOPUS (until May 2022); Central Cochrane Registry of Controlled Trials (The Cochrane Library) (until May 2022); MEDLINE (Ovid) until May 2022; EMBASE (Ovid); CINAHL (until May 2022); in addition to the reference list of included studies and other relevant data in addition to potentially eligible studies. The strategy comprised topic headings (MeSH) such as "Decompressive laparotomy," "traumatic brain injury," "Neurocritical care," and "intracranial hypertension," as well as text words associated with Booleans terms. The studies included randomized controlled trials (RCTs), Quasi randomized controlled studies, prospective and retrospective observational studies, series of cases or case reports that employed laparotomy as a therapy for intracranial hypertension. The Newcastle - Ottawa Quality Assessment Scale17) was used to assess the quality of research included; studies with a score of 9 were regarded to have good methodological quality (7 to 9 points). For observational studies, ratings in the range of 6 were considered Moderate Quality, whereas scores of 5 or less were considered Low Quality. The Case quality evaluation throughout CARE check list18) as 13 domains with 30 elements for report. A score of 25 to 30 was classified as High Quality, a score of 18 to 24 as Moderate Quality, a score of 16 to 18 as Low Quality, and a score of 15 or less as Very Low Quality. The following data were retrieved individually and separately: mortality, functional independence (modified Rankin scale 0 to 2, or Glasgow Prognostic Scale with a score of 4 or above), intracranial pressure value before and after Decompressive laparotomy, authors were contacted for missing data. Consultation by consensus helped to clear up any confusion. Statistical analysis was carried out using MEDCAL 19.3 software and the pooled rate of means for grouped data for prognosis evaluation. Because the number of included papers was minimal and this meta-analysis contained case reports, heterogeneity was not addressed.
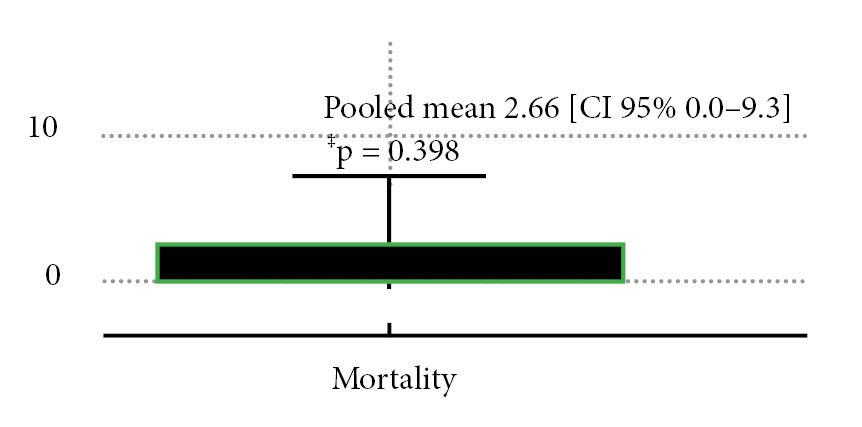
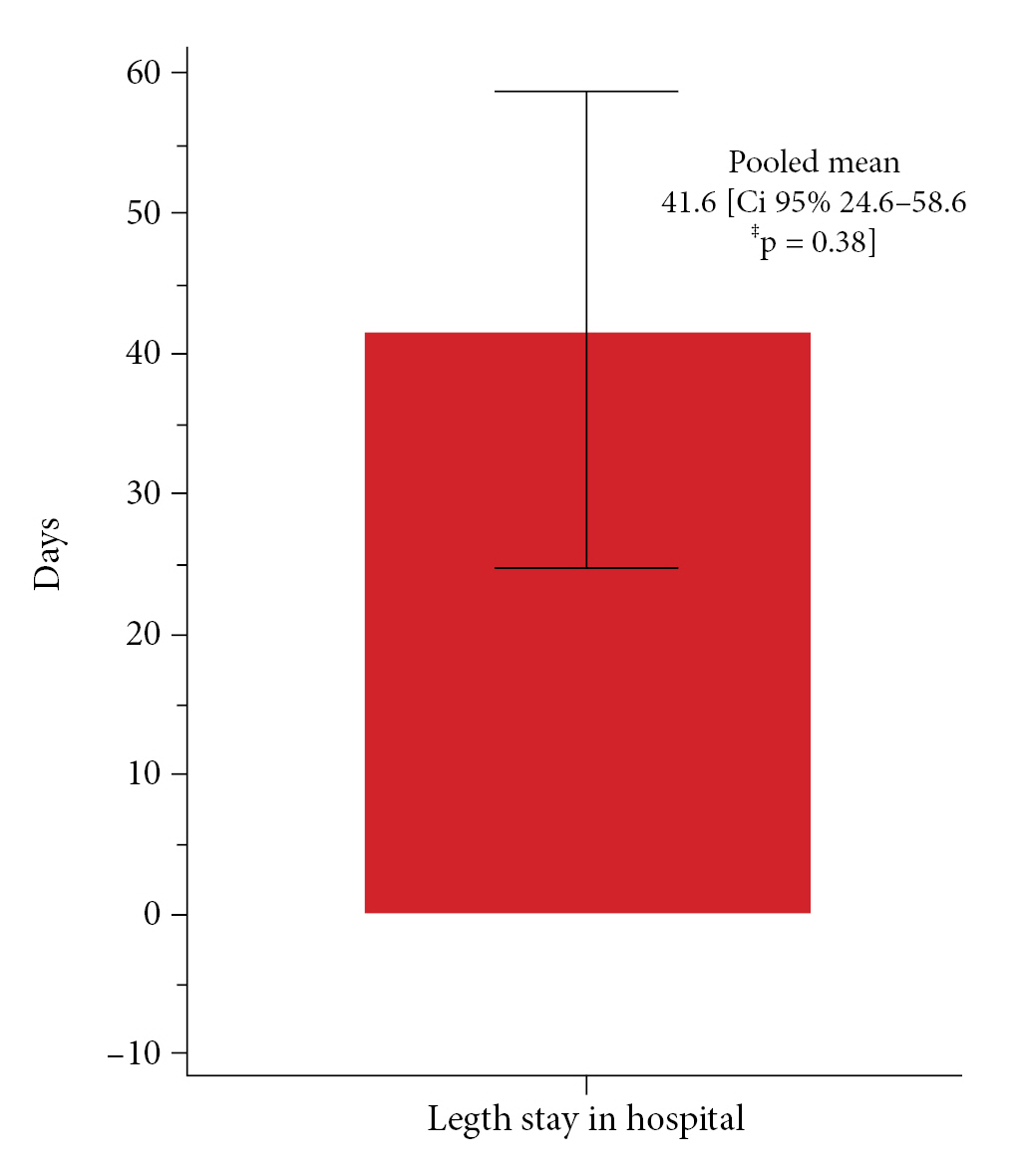
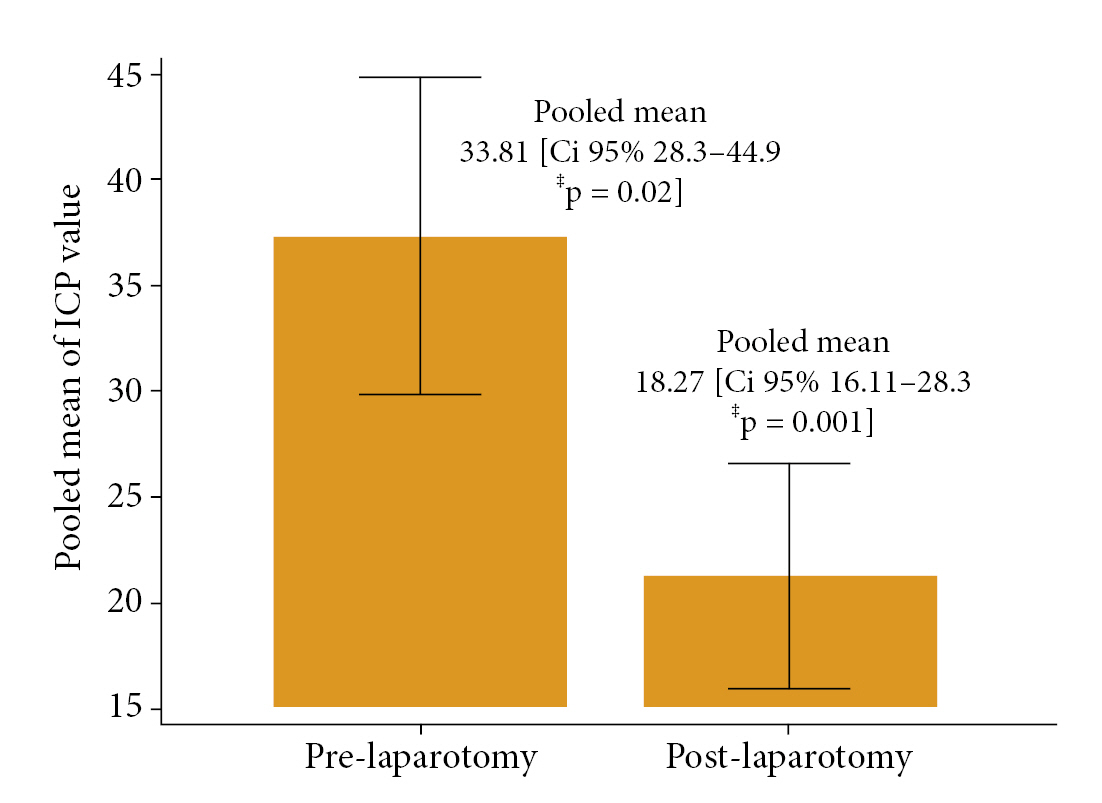
Following our technique of conducting a systematic search for information, 77 bibliographic citations were found. After deleting duplicates, just 50 remained. 50 were identified potentially eligible (based on title or abstract, or both), and complete texts were obtained; 40 were rejected since they were not trauma victims. Following a full text examination, 10 studies were examined for confidentiality: one is a narrative review, two do not contain traumatic brain injury, and one includes thoracic and neck trauma. Six studies were included for qualitative and quantitative analysis. Fig. 1 depicts two observational retrospective cohort studies and four case reports. Tables 1 and 2 illustrate the features of studies included9-14) and eliminated (with reasons)19-22). Among the six trials examined, 46 patients with TBI and intracranial hypertension were assessed and treated with hyperosmolar treatment and/or Decompressive Craniectomy with Decompressive laparotomy. Mortality was defined as death at the end of follow-up; no statistically significant results were identified among patients who underwent decompressive laparotomy, with a pooled mean of 2.66 deaths (Mean 2.66 CI95% 0.0-3.3 p = 0.398) (Fig. 2). The pooled mean of the days in this meta-analysis revealed a long hospital stay of 41.6 days (95% CI 24.6 to 58.6 p = 0.38) with no statistical significance (Fig. 3). After performing a decompressive laparotomy, the mean intracranial pressure drops to normal levels. Pre-laparotomy 33.8 mm Hg measured (95% CI 28.3 to 44.9 p = 0.02) and post-laparotomy 18.24 mm Hg measured (95% CI 16.11 to 28.3 p = 0.0001). All patients’ ICPs were assessed with an external ventricular shunt device (Fig. 4). The Glasgow Outcome Scale was used to assess neurological prognosis and functional competence. According to the findings, 8% of the patients were in a chronic vegetative state, 37.93% had severe disability, 33.45% had moderate disability, and the majorities (64.3%) were able to return to work with limitations, while 20.6% had mild disability or good functional recovery (Fig. 5). Only two observational studies were considered, Joseph et al. 12) and Scalea et al14), which received 5 and 6 points on the Newcastle Ottawa scale, respectively, indicating poor and intermediate quality. The quality of the included case reports was assessed using the CARE Check list. Armanious et al. 10) and Al-jehani et al. 9) are high quality case reports, meeting 28 and 27 quality criteria on the CARE list, respectively. Miglietta et al. 13) 22 met 22 out of 30 criteria, yielding a case report of intermediate quality.
Improving outcomes requires prompt care of intracranial after severe TBI1,2). Head elevation, sedation, osmotherapy, decompressive craniectomy, barbiturate coma, and therapeutic hypothermia are all listed as ways to regulate high intracranial pressure, either alone or in various combinations7). The feasibility of decompressive laparotomy has been investigated in selected patients with refractory intracranial hypertension12,13,21,22). The concept of decompressive laparotomy in situations of intractable intracranial hypertension is based on the little evidence that suggests intracranial, intra-thoracic, and intra-abdominal pressures are all connected9-14,19-22). It is postulated that increased intra-abdominal pressure causes cephalad diaphragm displacement, resulting in increased intrathoracic pressure and central venous pressure, which is then conveyed to the cerebral cavity via the venous system14,20,23,24). The authors suggested in a case report that a patient who had numerous traumas (including severe TBI) and underwent large transfusion developed refractory cerebral hypertension that responded to abdominal compartment syndrome laparotomy (ACS) 25-27). Other studies have found that individuals who received high-volume fluid resuscitation were more likely to develop ACS, and that in these cases, refractory intracranial may respond to surgical abdominal decompression25-27). Overall, the decision to pursue aggressive surgical surgery in instances of intractable intracranial hypertension requires careful consideration10,13,14). Decompressive laparotomy had been investigated as an alternative to decompressive hemicraniectomy in patients with bilateral disease necessitating bilateral hemispheric craniectomy or a bifrontal craniectomy, with the expectation that it would be a surgery with less overall morbidity9,14). In cases of recalcitrant cerebral hypertension, decompressive laparotomy must be performed with caution due to the significant morbidity and mortality9,10). To support the basic premise, writers developed methods to evaluate intraabdominal pressure and thereby connect the findings with measurements of intracranial pressure10).
Fig. 1.
Process of study selection. Flow chart of our search strategy and inclusion and exclusion criterial.
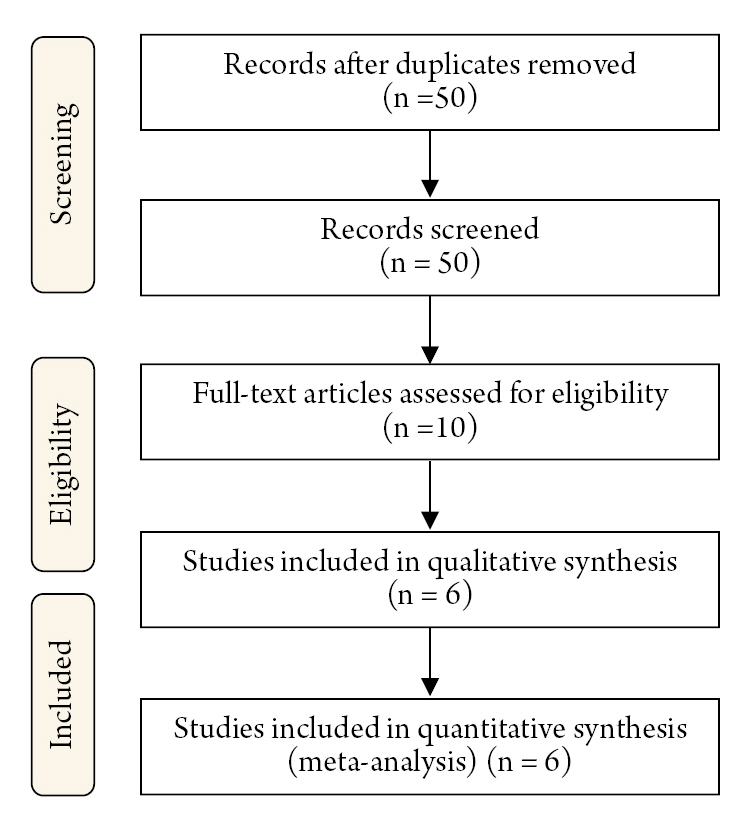
Table 1.
Characteristics of excluded studies
| Study | Type | N | Management of high intracranial pressure | ICP before laparotomy and post-laparotomy | Outcomes | Length Follow-up | Quality |
|---|---|---|---|---|---|---|---|
| Miglietta et al 200313) | Case report | 2 | Case 1 | Case 1 | Case 1 | In hospital | CARE |
| Hypertonic Saline solution 3%, barbiturate treatment and decompressive Craniectomy | Pre-laparotomy: 40±4 mm Hg | Glasgow Outcome scale: 5 | 22/30 | ||||
| Case 2 | Post-laparotomy | Length of stay in hospital: 17 | Moderate | ||||
| Hypertonic Saline solution 3% | 18±3 mm Hg | Outcome: Survival | |||||
| Case 2 | Case 2 | ||||||
| Pre-laparotomy: 47±4 mm Hg | Glasgow Outcome scale: 5 | ||||||
| Post-laparotomy | Length of stay in hospital: 30 | ||||||
| 22±3 mm Hg | Outcome: Survival | ||||||
| Joseph et al. 200412) | Observational retrospective | 17 | Hypertonic Saline solution 3% | Pre-laparotomy: 30±4 mm Hg | Mortality 6/17 | 6 months | NOS |
| Decompressive Craniectomy (2) | Post-laparotomy | Glasgow Outcome scale: 4±1 | 5/9 | ||||
| 17.5±3 mm Hg | Length of stay in hospital: 45±3 days | Low | |||||
| Scalea et al 200714) | Observational retrospective | 24 | Hypertonic Saline solution 3% and 7.5% | Pre-laparotomy: 28±11 mm Hg | Mortality 10/24 Glasgow Outcome scale: 3±2 | 1 year | NOS |
| Post-laparotomy | Length of stay in hospital: 29±16 days | 6/9 | |||||
| 19±10 mm Hg | Moderate | ||||||
| Dorfman et al 201111) | Case report | 1 | Hypertonic Saline solution 3% and Manitol | Pre-laparotomy: 35±5 mm Hg | Glasgow Outcome scale: 3 | 3 Months | CARE |
| Post-laparotomy | Length of stay in hospital: 47±5 | 28/30 | |||||
| 21±5 mm Hg | Outcome: Survival | High | |||||
| Armanious et al 201310) | Case report | 1 | Hypertonic Saline solution 3% and 7.5% | Pre-laparotomy: 41±5 mm Hg | Glasgow Outcome scale: 4 | 1 year | CARE |
| Post-laparotomy | Length of stay in hospital: 47 days | 28/30 | |||||
| 31±4 mm Hg | Outcome: Survival | High | |||||
| Al-jehani et al 20139) | Case report | 1 | Hypertonic Saline solution 3% and 7.5% | Pre-laparotomy:38±2 mm Hg | Glasgow Outcome scale: 4 | 1 year | CARE |
| Post-laparotomy | Length of stay in hospital: 64 days | 27/30 | |||||
| 20±4 mm Hg | Outcome: Survival | High |
Table 2.
Excluded studies with reason
| Excluded studies | Reason for exclusion |
|---|---|
| Lauerman et al 201421) | Is a Narrative review |
| Ertel et al 200020) | Assessment Abdominal and Pelvic trauma. The Traumatic brain injury was not assessed |
| Nagpal et al 200922) | Assessment hypoxic cerebral injury |
| Beucler et al 202219) | Included thoracic and neck trauma patients |
REFERENCES
1. Carney N, Totten AM, O'Reilly C, Ullman JS, Hawryluk GW, Bell MJ, et al. Guidelines for the management of severe traumatic brain injury, fourth edition. Neurosurgery 2017;80:6–15.



2. Brain Trauma Foundation; American Association of Neurological Surgeons; Congress of Neurological Surgeons; Joint Section on Neurotrauma and Critical Care, AANS/CNS; Carney NA, Ghajar J. Guidelines for the management of severe traumatic brain injury. Introduction. J Neurotrauma 2007;24 Suppl 1:S1–2.
3. Juul N, Morris GF, Marshall SB, Marshall LF. Intracranial hypertension and cerebral perfusion pressure: influence on neurological deterioration and outcome in severe head injury. The executive committee of the international selfotel trial. J Neurosurg 2000;92:1–6.
4. Polin RS, Shaffrey ME, Bogaev CA, Tisdale N, Germanson T, Bocchicchio B, et al. Decompressive bifrontal craniectomy in the treatment of severe refractory posttraumatic cerebral edema. Neurosurgery 1997;41:84–92; discussion 92-94.


5. Rutigliano D, Egnor MR, Priebe CJ, McCormack JE, Strong N, Scriven RJ, et al. Decompressive craniectomy in pediatric patients with traumatic brain injury with intractable elevated intracranial pressure. J Pediatr Surg 2006;41:83–87.


6. Sahuquillo J, Arikan F. Decompressive craniectomy for the treatment of refractory high intracranial pressure in traumatic brain injury. Cochrane Database Syst Rev 2006;(1):CD003983.
7. Hawryluk GWJ, Aguilera S, Buki A, Bulger E, Citerio G, Cooper DJ, et al. A management algorithm for patients with intracranial pressure monitoring: the Seattle International Severe Traumatic Brain Injury Consensus Conference (SIBICC). Intensive Care Med 2019;45:1783–1794.




8. Lazaridis C. Deciding under uncertainty: the case of refractory intracranial hypertension. Front Neurol 2020;11:908.



9. Al-Jehani HM, Hall JA, Maleki M. Decompressive laparotomy for treatment of refractory intracranial hypertension, thinking out of the box. Neurosciences (Riyadh) 2013;18:382–384.

10. Armanious M, Bacon LN, Harris J, George S, Goulbourne K, Danner OK, et al. Decompressive laparotomy for reduction of incessant increased intracranial pressure in the absence of abdominal compartment syndrome: a case report. Int J Case Rep Imag 2013;4:419–422.

11. Dorfman JD, Burns JD, Green DM, DeFusco C, Agarwal S. Decompressive laparotomy for refractory intracranial hypertension after traumatic brain injury. Neurocrit Care 2011;15:516–518.



12. Joseph DK, Dutton RP, Aarabi B, Scalea TM. Decompressive laparotomy to treat intractable intracranial hypertension after traumatic brain injury. J Trauma 2004;57:687–93; discussion 693-5.


13. Miglietta MA, Salzano LJ, Chiu WC, Scalea TM. Decompressive laparotomy: a novel approach in the management of severe intracranial hypertension. J Trauma 2003;55:551–554; discussion 554-555.


14. Scalea TM, Bochicchio GV, Habashi N, McCunn M, Shih D, McQuillan K, et al. Increased intra-abdominal, intrathoracic, and intracranial pressure after severe brain injury: multiple compartment syndrome. J Trauma 2007;62:647–56; discussion 656.


15. Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 2000;283:2008–2012.


16. Higgins, J.P., et al., Cochrane handbook for systematic reviews of interventions. 2019: John Wiley & Sons.
17. Wells, G., et al., Newcastle-Ottawa quality assessment scale cohort studies. University of Ottawa, 2014.
18. Gagnier JJ, Kienle G, Altman DG, Moher D, Sox H, Riley D; CARE Group. The CARE guidelines: consensus-based clinical case reporting guideline development. J Med Case Rep 2013;7:223.




19. Beucler N, Sellier A, Joubert C, Bernard C, Desse N, Esnault P, et al. Severe trauma patients requiring undelayable combined cranial and extra-cranial surgery: a proof-of-concept monocentric study. Mil Med 2022;187:1127–1135.



20. Ertel W, Oberholzer A, Platz A, Stocker R, Trentz O. Incidence and clinical pattern of the abdominal compartment syndrome after "damage-control" laparotomy in 311 patients with severe abdominal and/or pelvic trauma. Crit Care Med 2000;28:1747–1753.


21. Lauerman MH, Stein DM. Multicompartment management of patients with severe traumatic brain injury. Curr Opin Anaesthesiol 2014;27:219–224.


22. Nagpal S, Halpern CH, Sims C, Calland JF, Gracias VH, Schuster JM, et al. Decompressive laparotomy to treat intractable cerebral hypoxia. J Trauma 2009;67:E152–E155.


23. Citerio G, Vascotto E, Villa F, Celotti S, Pesenti A. Induced abdominal compartment syndrome increases intracranial pressure in neurotrauma patients: a prospective study. Crit Care Med 2001;29:1466–1471.


24. Maxwell RA, Fabian TC, Croce MA, Davis KA. Secondary abdominal compartment syndrome: an underappreciated manifestation of severe hemorrhagic shock. J Trauma 1999;47:995–999.


25. Bloomfield G, Saggi B, Blocher C, Sugerman H. Physiologic effects of externally applied continuous negative abdominal pressure for intra-abdominal hypertension. J Trauma 1999;46:1009–1014; discussion 1014-1016.


- TOOLS
-
METRICS

-
- 1 Crossref
- 2,451 View
- 75 Download
- Related articles in JNIC