Impact of Critical Care Registered Dietitian on Clinical Outcomes of Neurocritically Ill Patients
Article information
Abstract
Background
To investigate the impact of early nutrition intervention and a critical care registered dietitian on the outcomes of neurocritically ill patients.
Methods
Among neurosurgical patients admitted to the intensive care unit (ICU) in a tertiary hospital from January 2015 to December 2019, A critical care registered dietitian co-management was initiated on May 1, 2017. The primary endpoint was ICU mortality. Propensity score matching (PSM) was used to control selection bias and confounding factors.
Results
In this study, 1,386 patients were included. In the overall study population, nutrition was provided to 719 (51.9%) patients under the supervision of a registered dietitian. Early nutrition was performed for 356 (25.7%) patients. In the overall study population and the PSM adjusted population, rates of early parenteral nutrition (EPN) were higher in the groups managed by a registered dietitian than in the group without a registered dietitian (both p <0.001). In the overall and PSM adjusted population, the rates of ICU mortality, 28-day mortality, and in-hospital mortality were not significant different between two groups (all p>0.05), but the group managed by a registered dietitian had a shorter hospital stay than the group without a registered dietitian (both p<0.02). In the multivariable analysis of the overall population and PSM adjusted population, EPN showed an association with ICU mortality.
Conclusion
The rate of EPN utilization increased after the implementation of co-management with a critical care registered dietitian, and the use of EPN was associated with lower ICU mortality in neurocritically ill patients.
INTRODUCTION
Nutrition is a vital aspect of patient care, particularly for critically ill patients. Adequate nutrition support is essential for these patients to maintain their energy balance and achieve optimal outcomes1-3). In the neurocritical care setting, where patients often suffer from severe neurological injuries and require prolonged hospitalization, nutrition management becomes even more critical4-6). Studies have shown that early initiation of enteral nutrition and the involvement of a registered dietitian in the care team can improve clinical outcomes in critically ill patients7-9).
However, despite the potential benefits, there is still a significant variability in the delivery of nutrition therapy for critically ill patients, even among specialized units such as neurocritical care units10). The reasons for this variability are complex and multifactorial, but they may include differences in clinical practice patterns, staff knowledge and training, and resource availability5,11). Given the complexity of the factors that affect nutrition management in the neurocritical care setting, a multidisciplinary team approach that involves close collaboration between healthcare professionals with different expertise, such as neurosurgeons, neurointensivists, nurses, and dietitians, may be necessary to optimize nutrition management for these patients.
Therefore, in this study, we aimed to investigate the impact of early nutrition intervention and multidisciplinary team care that includes a critical care registered dietitian on the outcomes of neurocritically ill patients. We hypothesized that the involvement of a critical care registered dietitian in the neurocritical care team and the early initiation of enteral or parenteral nutrition would improve the clinical outcomes of neurocritically ill patients. We used propensity score matching to control for selection bias and confounding factors, and we assessed the outcomes of interest, including mortality, and length of hospital stay.
METHODS
Study population
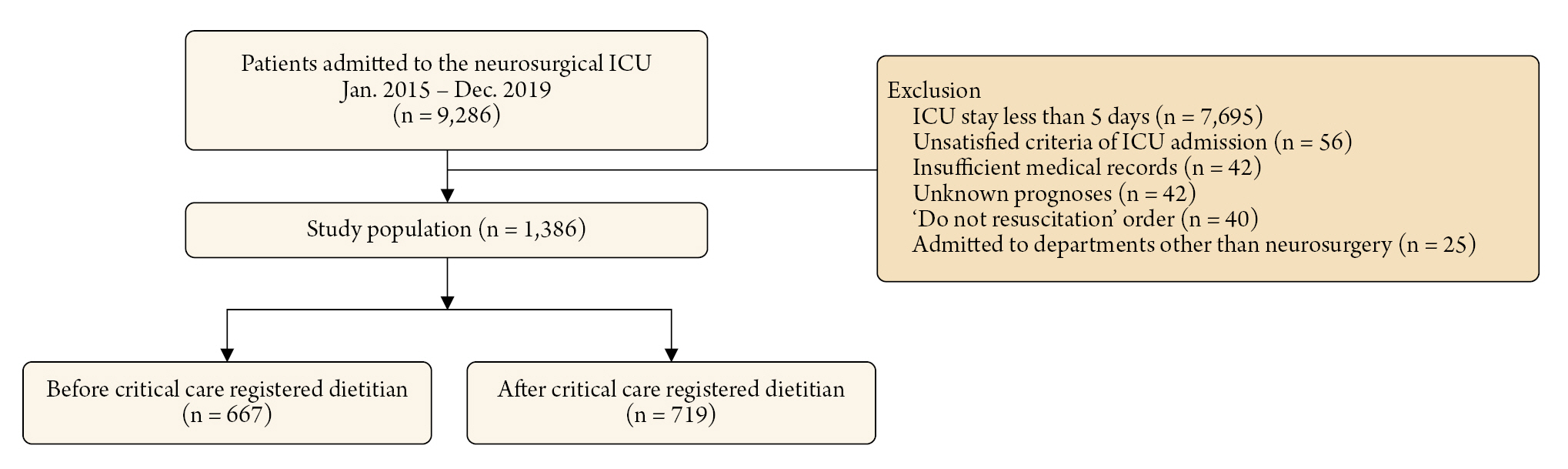
The study was approved by the Institutional Review Board (IRB) of Samsung Medical Center (No. SMC 2020-09-082) and patients' records were reviewed and published in accordance with the Declaration of Helsinki. Due to the retrospective nature of the study, the requirement for informed consent was waived by the IRB. We included patients who were hospitalized in the neurosurgical ICU for the management of neurocritical illness or for postoperative care after neurosurgery, as well as those who were hospitalized in the ICU for more than 3 days. Patients who had insufficient medical records, 'do not resuscitate' orders, were admitted to departments other than neurosurgery, or were transferred to other hospitals or had unknown prognoses were excluded from the study (Fig. 1).
Definitions and endpoints
In this study, baseline characteristics such as comorbidities, behavioral risk factors, ICU management, and laboratory data were collected retrospectively using Clinical Data Warehouse. Our center constructed a “Clinical Data Warehouse Darwin-C” designed for investigators to search and retrieve de-identified medical records from electronic archives.
A critical care registered dietitian co-management was initiated on May 1, 2017. The registered dietitian attended the weekly neurocritical care team meetings in person, and on days when not attending the meeting, she provided advice to the neurocritical care team on nutritional issues by phone after morning rounds. Patients who started enteral nutrition or parenteral nutrition within 72 hours of ICU admission were categorized as the early nutrition group. Early enteral nutrition (EEN) or early parenteral nutrition (EPN) was defined as the initiation of enteral nutrition or parenteral nutrition within 72 hours after ICU admission. The primary endpoint was ICU mortality. Secondary endpoint were 28-day mortality, in-hospital mortality and length of hospital stay.
Statistical analyses
Continuous variables are presented as means ± standard deviations, while categorical variables are presented as frequencies and proportions. Data were compared using Student's t-test for continuous variables and either the chi-square test or Fisher's exact test for categorical variables. To control for selection bias and confounding factors detected in this observational study, we employed several analysis methods, including propensity score matching (PSM)13). In the PSM analysis, each patient was matched with one control patient using the nearest neighbor matching method within calipers determined by the propensity score. A caliper width of 0.2 of the standard deviation of the logit of the propensity score was used for the matching14). We compared the balance of baseline covariates between nutrition groups by calculating the standardized mean difference (SMD)15). If PSM analysis successfully balanced the exposure groups, the standardized mean difference (SMD) should approach zero16). Therefore, SMDs less than 10% were considered appropriate for achieving balance between the two groups in this study. To evaluate whether there were differences in ICU mortality according to clinical variables, we performed multiple logistic regression with stepwise variable selection in the overall population and PSM population. We aimed to obtain results that corrected confounding through regression adjustment in the overall population. Furthermore, we performed doubly robust estimation to correct any potential biases that may still exist after PSM. All tests were two-sided and p values of less than 0.05 were considered statistically significant. All statistical analyses were performed with R Statistical Software version 4.0.2 (R Foundation for Statistical Computing, Vienna, Austria).
RESULTS
Baseline characteristics
A total of 9,286 patients were admitted to the neurosurgical ICU during the study period and 1,386 patients were included in the final analysis. In the overall study population, nutrition was provided to 719 (51.9%) patients under the supervision of a clinical dietitian (Fig. 1). Early nutrition was performed for 356 (25.7%) patients. Malignancy (61.8%) and hypertension (34.7%) were the most common comorbidities. Brain tumors (44.6%) and intracerebral hemorrhage (15.2%) were the most common reasons for ICU admission (Table 1). There were no significant differences between before and after clinical dietitian co-management except hypertension, APACHE2 score, and use of continuous renal replacement therapy, glycerin, and vasopressor (Table 1). In PSM adjusted population, there were no significant differences of clinical variables between two groups (Table 2).

Baseline characteristics and clinical outcomes according to co-management of critical care registered dietitian
Clinical outcomes and early nutrition
In the overall study population, early nutrition was at a similar frequency in both groups (28.1 % vs. 23.5%, p=0.068). However, the group managed by a registered dietitian had higher rate of EPN than the group without a registered dietitian (17.1% vs. 10.0%, p <0.001). In the PSM adjusted population, rate of EPN was also higher in the group managed by a registered dietitian than in the group without a registered dietitian (17.9% vs. 10.1%, p<0.001). In the overall study population and PSM adjusted population, the rates of ICU mortality, 28-day mortality, and in-hospital mortality were not significant different between two groups (all p>0.05), but the group managed by a registered dietitian had a shorter hospital stay than the group without a registered dietitian (both p<0.02) (Tables 1, 2).
In the multivariable analysis of the overall population, EEN (adjusted OR: 0.27, 95% CI: 0.09 – 0.68) and EPN (adjusted OR: 0.40, 95% CI: 0.18 – 0.82) showed an association with ICU mortality, whereas the presence of a registered dietitian (adjusted OR: 1.23, 95% CI: 0.76 – 2.00) did not demonstrate any significant association. Similar to the findings in the overall population, EPN was found to be significantly associated with ICU mortality (adjusted OR: 0.35, 95% CI: 0.12 – 0.86) in PSM adjusted population. However, neither EEN nor co-management with a registered dietitian showed any significant association with ICU mortality in PSM adjusted population (Table 3). In the PSM-adjusted population with a GCS below 13, there was no significant change in in-hospital mortality among those who received dietitian consultations (p=0.497). However, a significant reduction in the incidence of infections (p=0.007) and an enhanced early nutritional support (p=0.018) were observed.
DISCUSSION
In this study, we investigated the impact of early nutrition intervention and multidisciplinary team care that includes a critical care registered dietitian on the outcomes of neurocritically ill patients. Major findings of this study were as follows. First, approximately one-fourth of neurocritically ill patients received early nutrition, with about one-seventh of these patients receiving support in the form of EPN. Second, following the initiation of co-management with a critical care registered dietitian, there was an increase in the rate of EPN utilization. Third, the group that received management from a registered dietitian had a shorter hospital stay compared to the group that did not receive this service. Finally, in both the overall population and the population adjusted by PSM, multivariable analysis indicated a significant association between EPN and ICU mortality.
Registered dietitians are healthcare professionals specialized in nutrition and dietetics, possessing the credentials to assess, diagnose, and treat nutritional problems17). Their role encompasses a broad range of responsibilities, including the planning and implementation of medically recommended diets, patient education, and monitoring the effectiveness of dietary interventions17). In the neurocritical care area, the role of registered dietitians is particularly pivotal18). Neurological patients, whether due to traumatic brain injuries, strokes, or other neurodegenerative diseases, often present with unique nutritional challenges. These can include dysphagia, altered metabolic rates, and specific nutrient requirements or restrictions19). A registered dietitian in this context plays a critical role in ensuring that these patients receive adequate and appropriate nutrition to support brain health, promote recovery, and prevent further complications. Their expertise is crucial in designing individualized nutritional plans that account for the complex interplay between neurological status, metabolic demands, and nutrient availability. Thus, the collaboration between neurocritical care teams and registered dietitians can significantly enhance patient outcomes by addressing the intricate nutritional needs inherent in this population18).
In the management of neurocritically ill patients, the role of registered dietitian is particularly important20). Neurological disorders can lead to dysphagia, which can result in malnutrition and dehydration. In addition, these patients often require specialized diets to manage their conditions and prevent further complications21). Critical care registered dietitian can work closely with the neurocritical care team to assess the nutritional status of these patients, develop personalized nutrition plans, and monitor their response to nutrition therapy. Critical care registered dietitian can also provide recommendations for feeding modalities, such as enteral or parenteral nutrition, and work to prevent complications such as refeeding syndrome. The timely initiation of nutrition has been shown to improve patient outcomes, and registered dietitian can play an important role in developing and implementing personalized nutrition plans for neurocritically ill patients21). Overall, the involvement of registered dietitian in the care of critically ill neurological patients can improve outcomes, reduce complications, and ultimately contribute to their recovery.
In early stages of neurocritically ill patients, providing adequate nutritional support is crucial due to the hypermetabolic response that often follows brain injury12,22). Increased intracranial pressure can lead to sympathetic hyperactivation, which may have an impact on gastrointestinal dysfunction23-25). Furthermore, EEN on in neurocritically ill patients can elevate the risk of complications such as high gastric residual volume, delayed gastric emptying, and aspiration pneumonia11). Despite ongoing discussions about the ideal timing and method of feeding, a recent meta-analysis has demonstrated that EPN is more effective than EEN in reducing mortality rates and infectious complications, as well as improving outcomes in patients with traumatic brain injury during the acute gut-intolerant phase5,26).
This study is subject to several limitations, including the fact that it relied on a retrospective review of medical records and utilized data extracted from a Clinical Data Warehouse. The use of nonrandomized registry data in this study may have introduced selection bias into the results. This study is a type of before-and-after study, so when the registered dietitian initially began working with the neurocritical care team, there may have been a window period that should have been excluded from the analysis in order to minimize the risk of bias in the study. Nutritional support for neurocritically ill patients was occasionally administered using non-protocol methods. Finally, the distribution of neurosurgical diseases in our study population differed from that typically seen in a general neurosurgical ICU, with a particularly high proportion of patients with brain tumors.
CONCLUSION
Neurocritically ill patients can face challenges in receiving appropriate nutritional support due to issues like decreased consciousness, elevated intracranial pressure, and gastrointestinal dysfunction caused by excessive sympathetic nerve activity, distinguishing them from general intensive care patients. A critical care registered dietitian considers these unique characteristics of neurocritically ill patients to provide suitable nutritional support. This tailored approach could potentially improve the overall prognosis for these patients.
Notes
Ethics statement
The study was approved by the Institutional Review Board (IRB) of Samsung Medical Center (No. SMC 2020-09-082) and patients' records were reviewed and published in accordance with the Declaration of Helsinki. Due to the retrospective nature of the study, the requirement for informed consent was waived by the IRB.
Author contributions
Conceptualization: HK, HJK, JAR. Methodology: HJK, JAR. Data curation: HK, JAR, Writing – original draft: HK, JAR. Formal analysis: All authors.
Conflict of interest
There is no conflict of interest to disclose.
Funding
None.
Data availability
None.
Acknowledgements
We would like to express our gratitude to Suk Kyung Choo, the nursing director of the neurosurgical intensive care unit, for her valuable advice and insightful discussions. Additionally, we extend our thanks to all the nurses in the neurosurgical intensive care unit at Samsung Medical Center for their exceptional work.