 |
 |
- Search
| J Neurointensive Care > Volume 6(1); 2023 > Article |
|
Abstract
Background
Intravascular embolization is an effective treatment option for cases of trauma induced massive maxillofacial bleeding (MFB). Yet, a viable guideline for endovascular treatment of MFB has not been established. This article investigates on parameters to distinguish suitable candidates of endovascular embolization among trauma victims with MFB, and discusses factors related to clinical outcomes.
Methods
From January 2015 to December 2018, 24 massive MFB patients underwent tranas-femoral angiography, and 16 of them proceeded with endovascular embolization (embolization group) while the other 8 patients only received angiography as no extravasation was observed (non-embolization group). We compared laboratory values and clinical factors related to the massive blood loss between the embolization group and the non-embolization group.
Results
Compared with the non-embolization group, the patients of the embolization group had a trend of lower values in hemoglobin (7.9 ┬▒ 3.6 g/dL vs 11.6 ┬▒ 2.3 g/dL, p = 0.047), base excess (-14.73 vs -6.9, p = 0.002), and systolic & diastolic blood pressure (100.5mmHg vs 59.9mmHg, 66.0 mmHg vs 30.9mmHg, respectively, p < 0.05). The overall mortality rate was 66.7% (87.5% in the embolization group, 25% in the non-embolization group). In the embolization group, there was no significant difference in all clinical and laboratory values between survivors and non-survivors.
Life-threatening maxillofacial bleeding (MFB) accompanying hemodynamic instability is a rare but lethal condition which occupies 1.2%ŌĆō4.5% of traumatic facial injuries1-3). The primary managements for such destructive status include manual compression, nasal packing, and correction of coagulopathy4,5). When the first-line management fails, a trauma surgeon, neuro-interventionist, or an emergency physician may consider trans-arterial embolization (TAE) as the second-line therapy6,7). However, there are limited number of studies on trauma induced MFB, and the concurrent literatures lack reliable guidelines regarding in what condition intravascular embolization should be considered as a treatment option for MFB 7-9).
The treatment results of life-threatening MFBs are usually poor as the initial hemodynamic status of the patients are extremely unstable; previous articles reported the mortality rate of MFB as high as 35%7). The mortality rate is even higher for intractable cases that are not controllable with the conservative methods10). The primary physicians have to make a decision whether to proceed with transfemoral cerebral angiography (TFCA). However, there are a considerable number of MFB cases where no extravasation is observed in TFCA, and thus, unable to receive embolization8,11). TFCA, as an invasive, time-consuming procedure, may induce another threat to the patient when embolization turned out to be unavailable1,6). Further, studies on mortality related factors to help predict the prognosis of MFB patients after embolization are very limited. Such uncertainty leads to difficulties in making treatment decisions in situations of life-threatening MFBs. In this article, we report experiences with interventional managements of severe MFB in a single Level I trauma center. The purpose of our study is to distinguish potential beneficiaries of TFCA among traumatic MFB patients, and to analyze the factors associated with the mortality rate in life-threatening MFB.
This study was approved by the Institutional Review Board (CR 322143).We retrospectively investigated on patients with MFB who underwent TFCA from January 2015 to December 2018 in a single trauma center.
Immediately upon arrival, the victims of major facial injuries received primary managements including wound compression, nasal packing, fluid resuscitation and transfusion while undergoing focused assessment sonography in trauma (FAST) to rule out other hemorrhagic focuses. Then, clinical decision was made to proceed with TFCA when the case satisfied with the four of below criteria.
a. Bleeding continues even with conservative methods such as manual compression, nasal packing.
b. The main cause of unstable vital sign is evaluated as severe facial bleeding (FAST sonography reveals no active bleeding in internal organs).
c. Hemodynamic instability persists despite the use of 2L or more fluid therapy, transfusion, or vasopressor
d. Facial bleeding diminished at the moment of low blood pressure (BP), but bleeding becomes severe again after resuscitation.
As a Level I trauma center, the trauma team consisted of a trauma surgeon, an emergency medicine physician, and a neurosurgeon with neurointervention skills, together ready to promptly and efficiently manage the trauma patients. All the intervention procedures were performed in a hybrid operation room, which was always available in a five-minute distance from the ER.
The initial resuscitation was led by the emergency physician; essentially secured an arterial line for BP monitoring and central line for rapid infusion of fluid and vasopressor. At the same time, the angiography technicians got ready to operate the angiography. After portable monitoring devices set up, the patient was moved to the hybrid operation room. From the emergency room to the hybrid operation room, 2 nurses, 1 emergency medicine physician and 1 trauma surgeon of the trauma team accompanied the patient. The emergency medicine staffs monitored the vital signs during transportation and the procedures. TFCA was conducted by one neurosurgeon.
If extravasation of dye was visible on the angiographic image, TAE was performed. If no definite extravasation was seen, only cerebral angiography was performed and the examination was terminated. After all the procedure finished, the patient was moved to the trauma intensive care unit. An example case is illustrated in the Fig. 1.
To analyze differences between patients who showed extravasation in TFCA proceeded with embolization and those who didnŌĆÖt, the patients were classified into two groups: a group that proceeded to embolization (embolization group), and a group that ceased with angiography only (non-embolization group)
a. Clinical data; initial mentality, Glasgow coma scale (GCS), BP (initial, post-procedural), amount of transfusion, mortality rate as a final outcome.
b. Laboratory results; initial & post-procedural hemoglobin (Hb), pH, lactate, base excess
c. Time interval; from the time when trauma occurs or the time of arrival at the ER to the angiography suite
d. Angiographic findings; whether embolization was implemented, type of offender if any
Considering the small sample size, statistical tests were performed using StudentŌĆÖs t-test and the non-parametric Wilcoxon signed rank test of continuous variables using SPSS Statistics version 20.0 (Armonk, NY: IBM Corp.), and p-value less than 0.05 was considered statistically significant.
With the same maneuver, the all clinical and laboratory parameters mentioned above were analyzed again within the embolization group to investigate differences in survivors and non-survivors.
24 patients with massive MFB underwent TFCA and included in this study, whose demographics and the initial status shown on Table 1. The average time taken from the onset of trauma to facial angiography was 240 (ranging 120-360) minutes. The overall mortality rate was 66.7% (16/24).
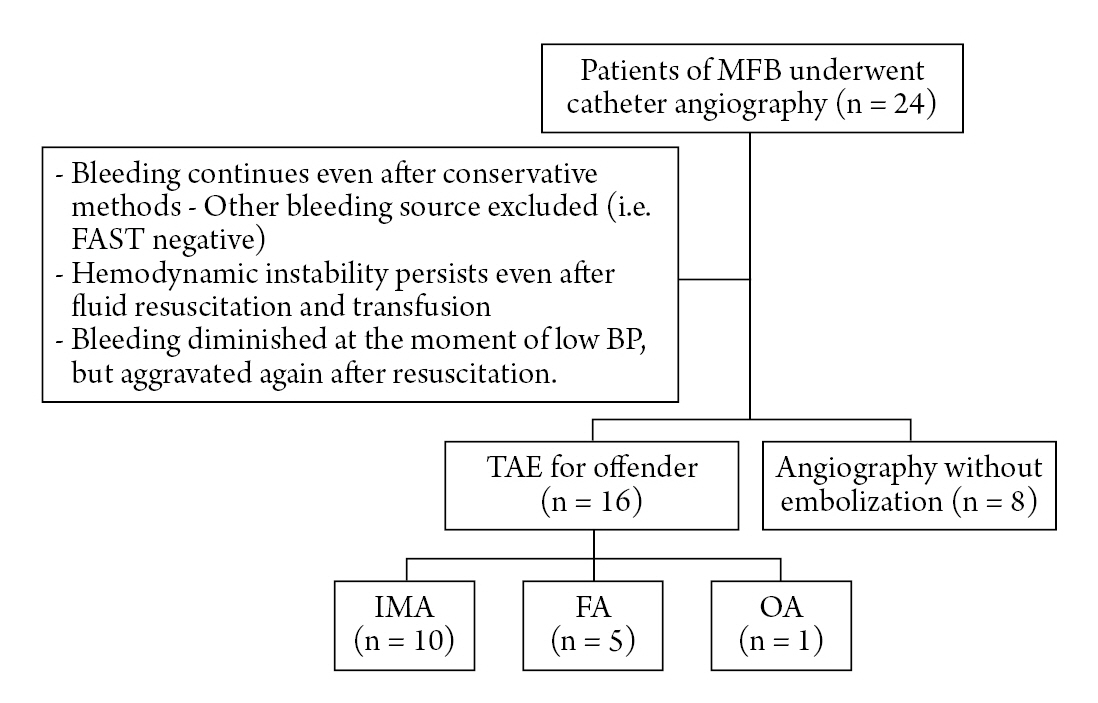
Among the 24 patients who received emergency angiography, 16 patients proceeded with TAE (Embolization group), and the other 8 patients ceased with only angiography as no available target artery was observed (Non-embolization group) (Fig. 2). Table 2 shows the hemodynamic, laboratory comparison between the two groups.
Regarding hemodynamics, the embolization group had a tendency of lower blood pressure (BP) initially, compared to the non-embolization group. Mean initial BP was significantly lower in the embolization group: systolic and diastolic blood pressure was 81.0 / 46.1 mmHg, 109.5/68.6 mmHg in the embolization group and the nonŌĆōembolization group, respectively (p = 0.011). After the procedure, in embolization group, both systolic and diastolic blood pressure were statistically different before and after the procedure (p = 0.044 & 0.010, systolic & diastolic); that is, the blood pressure significantly increased after the procedure in embolization group. The change in blood pressure before and after the procedure was also significantly different between the two groups (p = 0.044 & 0.011, systolic & diastolic).
In laboratory values, differences in shock related variables were observed as shown in Table 2. The mean initial plasma Hb level was 7.82 g/dL in the embolization group and 11.18 g/dL in the non-embolization group which showed a statistical difference (p = 0.001). Significantly low base excess values were found in the embolization group averaging -14.73, while average 6.9 base excess values were seen in the non-embolization group. (p = 0.013). However, pH and lactate showed no statistical significance (p = 0.358, 0.953 respectively). Initial GCS was higher in the non-embolization group (average 7.38), compared with the embolization group (average 4.19) (p=0.003). Time intervals from trauma to angio-suite, age, gender ratio were not significantly different between the two groups. The mortality rate of the embolization group was 87.5% (n=14/16), which was significantly higher than the non-embolization group (25%, n= 2/8) (p= 0.002).
The same parameters were reviewed to see differences between survivors and non-survivors within the embolization group, and no statistically significant difference was observed (Table 3).
In this study, we ultimately aimed to distinguish the candidates for trans-arterial embolization among the massive MFB patients. We investigated on the features found in the subgroup of patients with active arterial bleeding, who subsequently underwent the embolization, which were statistically different from the features shown by the other subgroup with the angiographic findings of only venous or bone bleeding. Our data analysis demonstrated that the parameters of the hemodynamic laboratory results were significantly different between the above two groups. Taken together, we believe that the results of this study are valuable that some critical clues can be obtained from patientsŌĆÖ clinical features which can help determine whether the patients need an emergent angiographic intervention and embolization or not.
The injuries resulting life-threatening traumatic maxillofacial bleeding often involve high kinetic energy transfer, for example, a traffic accident1,12). Such conditions create difficulties in airway management, and are related to high risk of concomitant injuries including internal organ bleedings. Even with preemptive and active managements, mortalities are often unavoidable in traumatic intractable maxillofacial bleeding12,13). Primary treatments, such as tight nasal packing or tamponade using balloon catheter, may be useful, but often insufficient5).
Therapeutic percutaneous embolization in maxillofacial bleeding has been developed mainly for intractable epistaxis since it was first reported by Sokoloff, et al. 3,14). One advantage of the catheter angiography in traumatic MFB is that it offers a viable treatment option even for hemodynamically unstable patients to whom general anesthesia may induce another threat. The relatively short procedure time is another superiority over more invasive treatment options. Considering the high rates of co-morbidities, accessibility to intrathoracic or intra-abdominal vasculature with a single transfemoral entry is another strength of the catheter angiography7).
Previous authors have proposed treatment guidelines and management algorithms in intractable life-threatening massive maxillofacial bleeding7,9). Based on the views of these authors, the indications for angiographic embolization can be briefly summarized as when bleeding is uncontrollable with conservative managements. However, in some cases, TFCAs do not show signs of active arterial bleeding thus embolization is unavailable11). This study further investigated on differences in clinical or laboratory values between those who showed extravasation in TFCA and those did not.
In Table 2, it was confirmed that the initial hemoglobin and base excess were lower in the embolization group than in the non-embolization group. Although other indicators were statistically insignificant, it can be interpreted that the initial hemodynamic status was more unstable in the embolization group. When comparing the clinical and laboratory values between the embolization and non-embolization group, some significant differences were observed. Initial systolic and diastolic blood pressure were significantly lower in the group where embolization was possible, suggesting that overt arterial bleeding had a relatively large amount of blood loss. After the procedure, the blood pressure of the embolization group became higher than before the procedure, whereas the blood pressure of the non-embolization group was lowered after the procedure; the differences were statistically significant. Such difference suggests effectiveness and necessity of embolization in proper cases, as well as the potential risk of the invasive angiography when embolization is not available and hemodynamic instability continues. Taken together, it can be carefully estimated that the embolization group had more severe hypovolemic status due to blood loss, which can be improved by embolization. Our results suggest initially lower blood pressure, hemoglobin and base-excess values are possible indicators of the potential beneficiaries of facial embolization among MFB patients. To support this idea and to determine cut-off values, more profound researches are demanded.
According to the previous studies, the major offenders of MFB are the internal maxillary artery (IMA) or the intraosseous branches of external carotid artery (ECA). Facial, angular, lingual, occipital, superior thyroid, middle meningeal, sphenopalatine, and the descending palatine arteries are possible candidates of extravasation8,15). In this study, IMA was reported as the most prevalent offender. (9/16, 56.3%, Table 1) accordant with the previous reports.
Liao, et al reported the clinical success rate of embolization in severe oronasal bleeding cases is as high as 79.4%7). In this study, all patients who underwent embolization succeeded in clinical hemostasis. Liao et al reported that higher GCS score (Ōēź8) and less extensive systemic injury, represented by Injury severity scale(ISS) Ōēż32 were related to higher survival rate8). Kuan et al. suggests that the survival of patients with successful TAE is associated with severity of trauma and concomitant brain injury16). In our study, the overall mortality rate was total 66.7% (16/24), 25% (2/8) in the non-embolization group, and 87.5% (14/16) in the embolization group. Arterial extravasation requiring embolization on angiography demonstrates more blood loss, and as the clinical outcome indicates, it is related to more severe injuries or more fatal status than when there was no such findings. As these unfavorable results show, embolization often fails to contribute to effective reduction of mortality rate even when successfully done.
However, according to the theory of traumatology, hypovolemic shock and severe brain injuries are the main cause of death within a few hours, referred as the second peak of trimodal distribution for mortality17). Intensive hemostasis is essential during this period. In MFB patients, to achieve hemostasis in situations where conservative managements are insufficient, embolization is currently the most viable alternative5,7). There were patients who showed immediate recovery in blood pressure after embolization, e.g. the patient in Fig. 1, who dramatically recovered from the natural course of the disease. The unfavorable result may not merely suggest the ineffectiveness of embolization in MFB; rather it proposes the necessity of viable guidelines to reduces the time from trauma to angio-suit and to facilitate the embolization process.
The point that should not be overlooked during the procedure is that, when systolic BP is 60 or less, bleeding stops grossly due to collapse of ECA branch vessels. If there is a response to treatment such as massive fluid resuscitation, transfusion or use of inotropic agents, bleeding occurs again. Therefore, caution should be taken when making judgments on such temporary pause of bleeding; the patients should not be excluded from the active treatment group even when bleeding seems to diminish.
This study carries several limitations; the statistical power is low with the small number of target patients in a single-institution study. Disadvantages of retrospective study are also present in this study. The past medical histories of the patients are not considered, sparing the effect of such status in clinical outcomes for the future studies. Despite the limitation of this study, we would like to share our experience in hoping to set up future evidence-based guidelines of facial artery interventions in order to improve the prognosis of severe maxillofacial injuries.
This study suggests initial hemoglobin and base-excess as possible indicators to distinguish the potential beneficiaries of facial embolization among MFB victims. However, it failed to find the viable prognosis factors to predict the clinical outcome of the embolization. Larger-scale prospective studies are needed in the future.
Fig.┬Ā1.
Angiographic findings and embolization in MFB patient.
62 year-old male, a victim of in-car TA, arrived in our trauma center 4 and a half hours after the trauma. The initial blood pressure was 64/24, Hb was 6.4. It took 40 minutes to make the decision to proceed with TFCA, and another 40 minutes until the puncture of the femoral artery. The embolization procedure required an hour. After the procedure the patient was moved to ICU. He survived and recovered from the injury. (A, B) angiography before embolization (AŌĆōAP view, BŌĆōlateral view, leakage area indicated by a red arrow), presenting leakage from buccal artery, which is a branch of internal maxillary artery. (C, D) microcatheter approach and microselection of target vessel. Implementation of embolization (E) and angiography after embolization (F) no leakage after embolization seen.
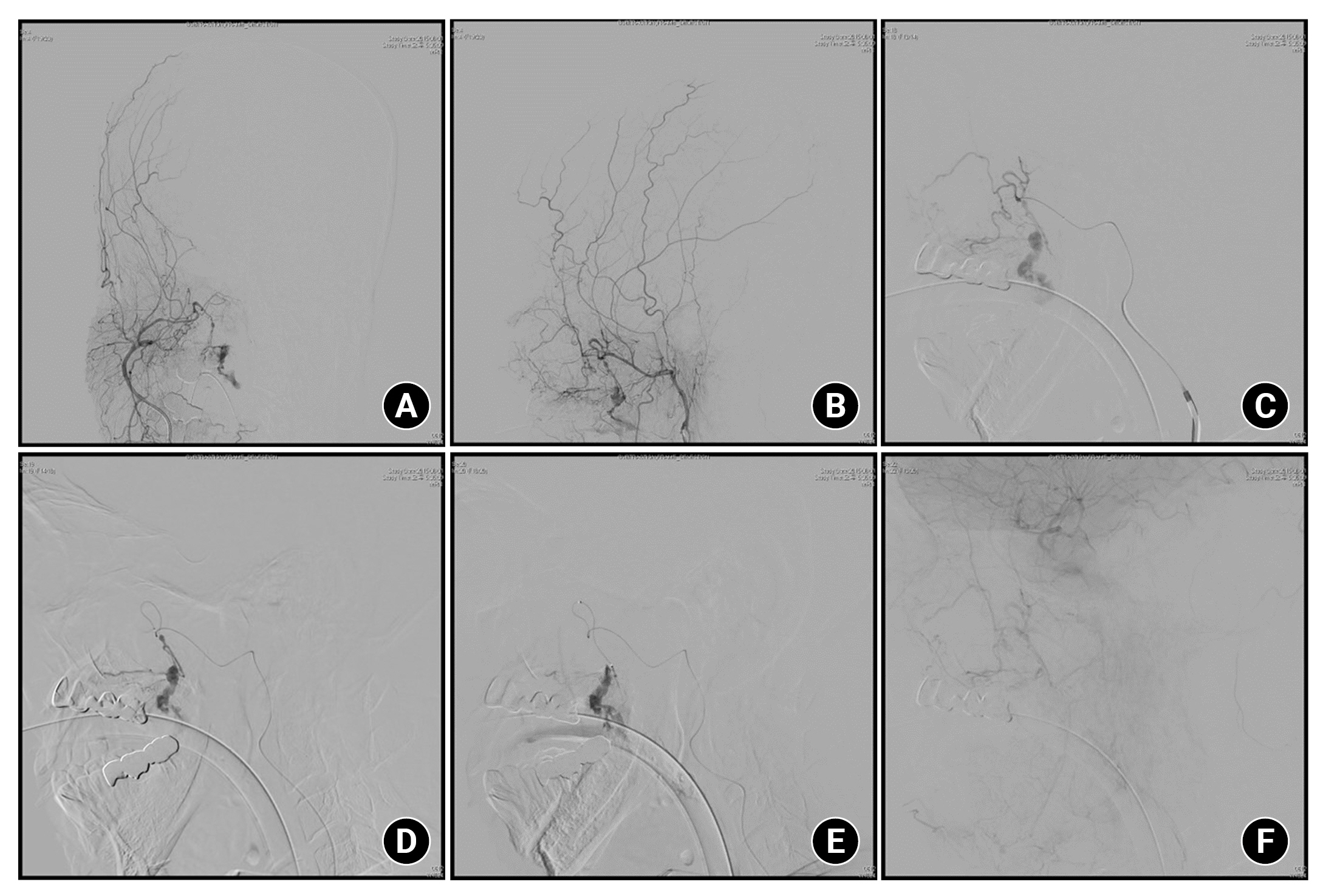
Fig.┬Ā2.
Flowchart classifying patients into the two groups, embolization and non-embolization group.
MFB: Maxillofacial bleeding, TAE: Transarterial embolization, IMA: Internal maxillary artery, FA: Facial artery, OA: Ophthalmic artery.
Table┬Ā1.
Demographics and initial status of the patients with massive maxillofacial bleeding
Table┬Ā2.
Comparison between the embolization group and non-embolization group
| Embo group (n=16, 67%) | NonŌĆōembo group (n=8, 33%) | pŌĆōvalue | |
|---|---|---|---|
| Age (years) | 45.94 (16ŌĆō69) | 59.75 (42ŌĆō77) | 0.073 |
| Initial GCS | 4.13 (3ŌĆō7) | 7.5 (4ŌĆō12) | 0.003* |
| Initial SBP (mmHg) | 81.06 (40ŌĆō140) | 109.5 (72ŌĆō140) | 0.020* |
| Initial DBP (mmHg) | 46.13 (20ŌĆō90) | 68.63 (45ŌĆō90) | 0.008* |
| Initial Hb (g/dL) | 7.82 (5.5ŌĆō11.6) | 11.18 (7.5ŌĆō14) | 0.001* |
| Initial PH | 7.15 (6.98ŌĆō7.29) | 7.21 (6.8ŌĆō7.45) | 0.358 |
| Initial Lactate (mmol/L) | 5.59 (1.4ŌĆō10.28) | 5.68 (1.95ŌĆō11.6) | 0.953 |
| Initial BE (mmol/L) | ŌĆō13.84 (ŌĆō20.2 to ŌĆō5.9) | ŌĆō8.01 (ŌĆō15.8ŌĆō1.1) | 0.014** |
| Time interval from | 238.71 (57ŌĆō420) | 243.75 (100ŌĆō540) | 0.928 |
| trauma to angioŌĆōsuite (mins) | |||
| PostŌĆōprocedural SBP (mmHg) | 103.56 (42ŌĆō164) | 104.38 (96ŌĆō112) | 0.950 |
| PostŌĆōprocedural DBP (mmHg) | 59.88 (32ŌĆō101) | 57.75 (46ŌĆō66) | 0.783 |
| Change in SBP** (mmHg) | 22.5 (ŌĆō77ŌĆō60) | ŌĆō5.13 (ŌĆō30ŌĆō28) | 0.044* |
| Change in DBP** (mmHg) | 13.75 (ŌĆō53ŌĆō45) | ŌĆō10.88 (ŌĆō37ŌĆō1) | 0.011* |
| Mortality rate | 87.5% | 25.0% | 0.002* |
Table┬Ā3.
Comparison between the survival group and expired group
REFERENCES
1. Bynoe RP, Kerwin AJ, Parker HH 3rd, Nottingham JM, Bell RM, Yost MJ, et al. Maxillofacial injuries and life-threatening hemorrhage: treatment with transcatheter arterial embolization. J Trauma 2003;55:74ŌĆō79.

2. Liu WH CY, Hsieh CT, Lin EY, Chung TT, Ju DT. Transarterial embolization in the management of life-threatening hemorrhage after maxillofacial trauma: a case report and review of literature. Am J Emerg Med 2008;26:516.e3-e5.
3. Sokoloff J, Wickbom I, McDonald D, Brahme F, Goergen TC, Goldberger LE. Therapeutic percutaneous embolization in intractable epistaxis. Radiology 1974;111:285ŌĆō287.


4. Harris T, Rice S, Watts B, Davies G. The emergency control of traumatic maxillofacial haemorrhage. Eur J Emerg Med 2010;17:230ŌĆō233.


5. Lee W, Shim YS, Chung J. Endovascular treatment to stop life-threatening bleeding from branches of the external carotid artery in patients with traumatic maxillofacial fracture. J Cerebrovasc Endovasc Neurosurg 2016;18:83ŌĆō89.




6. Dar P, Gupta P, Kaul RP, Kumar A, Gamangatti S, Kumar S, et al. Haemorrhage control beyond Advanced Trauma Life Support (ATLS) protocol in life threatening maxillofacial trauma - experience from a level trauma centre. Br J Oral Maxillofac Surg 2021;59:700ŌĆō704.


7. Chen YF, Tzeng IH, Li YH, Lo YC, Lin WC, Chiang HJ, et al. Transcatheter arterial embolization in the treatment of maxillofacial trauma induced life-threatening hemorrhages. J Trauma 2009;66:1425ŌĆō1430.


8. Liao CC, Hsu YP, Chen CT, Tseng YY. Transarterial embolization for intractable oronasal hemorrhage associated with craniofacial trauma: evaluation of prognostic factors. J Trauma 2007;63:827ŌĆō830.


9. Noy D, Rachmiel A, Emodi O, Amsalem Y, Israel Y, Nagler RM. Transarterial embolization in maxillofacial intractable potentially life-threatening hemorrhage. J Oral Maxillofac Surg 2017;75:1223ŌĆō1231.


10. Komiyama M, Nishikawa M, Kan M, Shigemoto T, Kaji A. Endovascular treatment of intractable oronasal bleeding associated with severe craniofacial injury. J Trauma 1998;44:330ŌĆō334.


11. Yuan KC, Wong YC, Lin BC, Kang SC, Liu EH, Hsu YP. Negative catheter angiography after vascular contrast extravasations on computed tomography in blunt torso trauma: an experience review of a clinical dilemma. Scand J Trauma Resusc Emerg Med 2012;20:46.




12. Scheyerer MJ, Doring R, Fuchs N, Metzler P, Sprengel K, Werner CML, et al. Maxillofacial injuries in severely injured patients. J Trauma Manag Outcomes 2015;9:4.




13. Down KE, Boot DA, Gorman DF. Maxillofacial and associated injuries in severely traumatized patients: implications of a regional survey. Int J Oral Maxillofac Surg 1995;24:409ŌĆō412.


14. Strach K, Schrock A, Wilhelm K, Greschus S, Tschampa H, Mohlenbruch M, et al. Endovascular treatment of epistaxis: indications, management, and outcome. Cardiovasc Intervent Radiol 2011;34:1190ŌĆō1198.



15. Cogbill TH, Cothren CC, Ahearn MK, Cullinane DC, Kaups KL, Scalea TM, et al. Management of maxillofacial injuries with severe oronasal hemorrhage: a multicenter perspective. J Trauma 2008;65:994ŌĆō999.


- TOOLS






