Cerebrospinal fluid (CSF) hypovolemia may occur spontaneously or after neurosurgical procedures. A spontaneous form of CSF hypovolemia have also known as spontaneous intracranial hypotension and usually take chronic and/or benign clinical course8). The other form of CSF hypovolemia is postoperative and often show problematic acute exacerbations during recovery from anesthesia or critical care except intraoperative therapeutic extensive CSF removal18) in some particular conditions. The pathophysiologic mechanisms, though not clearly demonstrated, of these acute deteriorations which the most close pathomechanism have been seemed to have a considerable consensus among many interested neurosurgeons, have been described separately in a number of case reports and case series1-13,15-17,19,21).
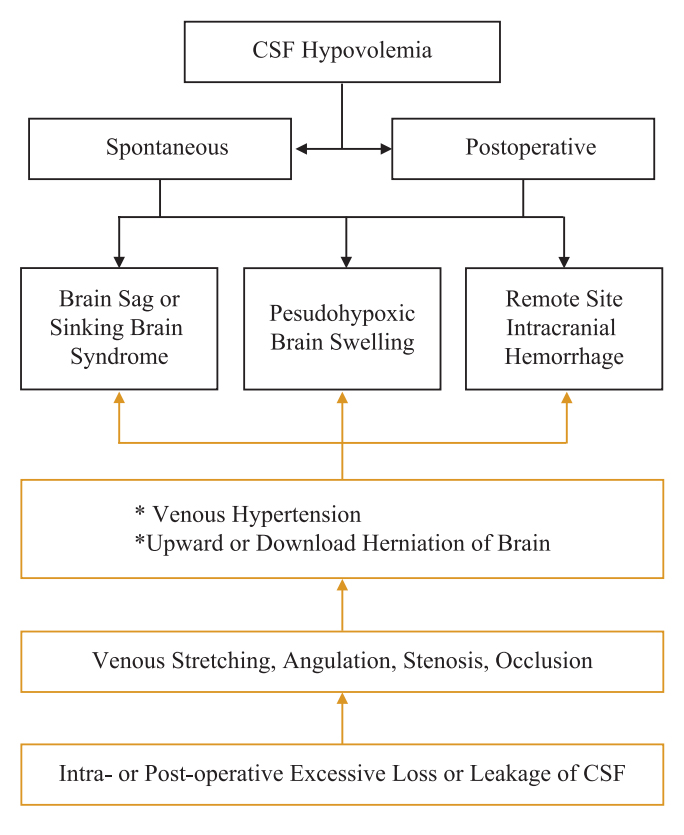
A comprehensive description, however, for clinical entities of postoperative CSF hypovolemia is almost rare until lately. Also, the terminologies related to postoperative CSF hypovolemia have not been uniformly standardized yet. The aim of this brief review of literatures is attempt to settle and analyze postoperative CSF hypovolemia comprehensively. As a postoperative complication, both the cranial and spinal16)surgeries, CSF hypovolemias might have been expressed in three different clinical types of phenomena; 1) brain sag, 2) pseudohypoxic brain swelling (PHBS), 3) remote site hemorrhage. Basically, these three clinical phenomena do not have any new theoretical concept. The author’s proposed classification and pathomechanism for these phenomena is shown in Fig. 1.
Above three types of clinical entities may have, essentially identical pathophysiologic mechanisms such as venous stretching, angulation, occlusion, or disturbed intracranial venous return to heart then venous hypertension, and may arise from the intra- or post-operative excessive loss of CSF via diverse routes including subarachnoid cisternal spaces, lamina terminalis, extraventricular drain, lumbar drain or puncture, subgaleal or epidural negative vacuum drain, or traumatic fractures of the skull base. And they also may have similar symptoms and signs whether benign or malignant form although their radiologic characteristics are quite distinct one another. In the management for these three clinical phenomena, the general principles are fundamentally same. That is, flat or Trendelenberg positioning of the patient and prevention of further CSF loss. Of course, detailed methods of treatment for each type of this clinical condition by the postoperative CSF hypovolemia can be exceedingly different.
The brain sagging, also called 'sinking brain syndrome5) is typically mild, and an upright positional headache is the most common presenting symptom. Other complaints such as nausea, vomiting, vertigo and visual disturbance may be subtle. Mild symptomatic brain sagging tends to recover spontaneously without any intervention except a few cases that may need the patients flat position for some time with or without epidural blood patches. Some brain saggings, especially immediate postoperative, may develop serious symptoms and signs such as coma with abnormal pupillary reflexes1,5-7,15). Diagnostic criteria for severe brain sagging by Komotar et al.10) are as followings; 1) clinical signs of transtentorial herniation, 2) head computed tomography (CT) scans revealing effacement of the basal cisterns with an oblong brainstem, 3) improvement of symptoms and/or signs upon placing the patient in the Trendelenberg position. In those circumstances, early detection and identification of brain sagging then Trendelenberg positioning, with primary cause management to prevent further CSF loss is mandatory. This management policy is extremely significant to arrest progression to irreversible neurologic deficits or death and to promote whole recovery.
PHBS, relatively newly coined and defined term, may be also caused by excessive CSF loss, especially through the subgaleal or epidural negative pressure suction drain19). And intraoperative CSF drainage may contribute to this complication. Variable degree of severity for PHBS can occur, although majority of PHBS cases are found to be grave neurologic deficits including not awakening from anesthesia, unreactive mydriasis, generalized seizure in uneventful elective neurosurgery19,20). This prevalence of critical severity especially, before the report by Van Roost et al.19), may be insufficient understanding of this phenomenon. Mild to moderate degree of PHBS may occur presenting abnormal mental status, signs of abnormal brainstem function, and etc, Typical imaging characteristics are diffuse brain swelling particularly involving bilateral basal ganglia and thalami on head CT or magnetic resonance images (MRI). Angiographic findings are commonly non-specific and may demonstrate only a slow circulation time by microcirculatory disturbance from diffuse brain swelling19,20). Principles of management are almost conclusive i.e., prevention of further CSF loss, Trendelenberg positioning, reduction of increased intracranial pressure. The prognosis of PHBS is variable, and usually depends on the time of correct diagnosis and treatment, then may be fatal or may show complete recovery19).
Remote site hemorrhage is the most repeatedly reported postoperative complication among three clinical phenomena due to postoperative CSF hypovolemia as mentioned earlier2,4,8,12,21). By definition, remote site hemorrhage is bleeding at a location or locations distant from the site of original surgery21). Although the first report was after supratentorial craniotomy it can occur after supra- or infra-tentorial surgery especially in sitting position3), burr hole trephination4), or spinal surgery20) i.e., neurosurgery of almost all kinds. Its prevalence is rather wide-ranging, from 0.2 to 4.9% after different kinds of neurosurgery2-4,8,12,21). Many hypotheses have been advocated and published for decades though the exact pathophysiologic cause has not been fully revealed yet. Radiologic findings are often non-specific except remote site intracranial hemorrhage in epidural, intracerebral, or cerebellar, which may appear solitary or multiple on head CT and/or MRI. Once such a adverse event develop it can become fatal. Surely, perfect restoration from neurologic deterioration after conservative management or asymptomatic cases are also possible2-4,8,12,16,17,21).
More recently, remote site hemorrhages have been published after successful endovascular treatment of cerebral aneurysms14). The suggested mechanisms of this complication have been far from the CSF hypovolemia, and are beyond the scope of the author’s discussion.
In summary, it is very crucial for neurosurgeons to remember that 1) most CSF hypovolemias after neurosurgery are probably unnoticed, and thus much underrated. 2) we, neurosurgeons always consider the possibility of above three clinical phenomena for differential diagnosis in case of neurologic deterioration after uneventful neurosurgical procedure. 3) prevention, although limited, of excessive loss of CSF perioperatively may be the best way to treat complications from postoperative CSF hypovolemia. Clear verification of the root pathomechanisms for these unanticipated and tough complications would create further investigations.