|
 |
- Search
| J Neurointensive Care > Volume 6(2); 2023 > Article |
|
Abstract
This case report addresses pharyngeal perforation, an uncommon complication after anterior cervical discectomy and fusion (ACDF). A 78-year-old male, who initially presented with quadriparesis, underwent ACDF. Post-surgery, the porridge he consumed was observed in the drain tube, leading to complications such as respiratory distress and fever. An emergency exploratory surgery was performed, and a suspected pharyngeal perforation was identified and treated with primary repair and sternocleidomastoid flap. Through thorough post-operative observation, we identified critical signs requiring immediate intervention, allowing for a successful recovery without additional complications. This report emphasizes the importance of early detection and intervention for complications following ACDF, providing valuable insights for clinical practice in neurosurgical intensive care.
Anterior cervical discectomy and fusion (ACDF) remains the prevailing standard for treating degenerative cervical myelopathy, especially when one or two-level herniated discs are present. Despite its efficacy, the anterior approach associated with ACDF can lead to certain complications. Dysphagia and hoarseness are most common1), but more severe complications could arise. One severe, though rare, complication includes the inadvertent perforation of the cervical esophagus or hypopharynx. Such perforations are life-threatening and present a significant risk of descending mediastinitis. The severity of these complications is further highlighted by the challenges in managing infections and the uncertainty in the resulting cervical alignment deformations2). Hence, when considering post-operative management from a critical care medicine perspective, it is imperative to acknowledge that these complications necessitate immediate surgical intervention. This report outlines our experiences, emphasizing the significance of early detection and appropriate intervention following pharyngeal injuries after anterior spinal surgery.
A 78-year-old male presented to our institution with a six-month progressive history of quadriparesis. Preoperatively, the patient exhibited motor grade 3 strength in the right upper and lower limbs and motor grade 2 strength in the left upper and lower limbs. Preoperative cervical magnetic resonance imaging (MRI) demonstrated cord compression attributed to herniated nucleus pulposus (HNP) at the C3-4 level (Fig. 1). Consequently, ACDF was performed at this level.
The intraoperative examination was unremarkable. Adhering to standard protocol, oral feeding commenced on the first post-operative day. However, the patient subsequently reported persistent coughing during meals and exhibited a fever of 38.1°C four hours after oral intake. Initially, this was considered a post-operative physiological fever and was closely monitored. The following day, a purulent, cloudy discharge was noted from the drainage catheter removal site (Fig. 2). This prompted the immediate administration of antibiotics (Vancomycin, Ceftriaxone) and intensified patient monitoring. Subsequent respiratory distress reduced oxygen saturation to 80%, and a chest X-ray identified pneumonia (Fig. 3), necessitating urgent intubation.
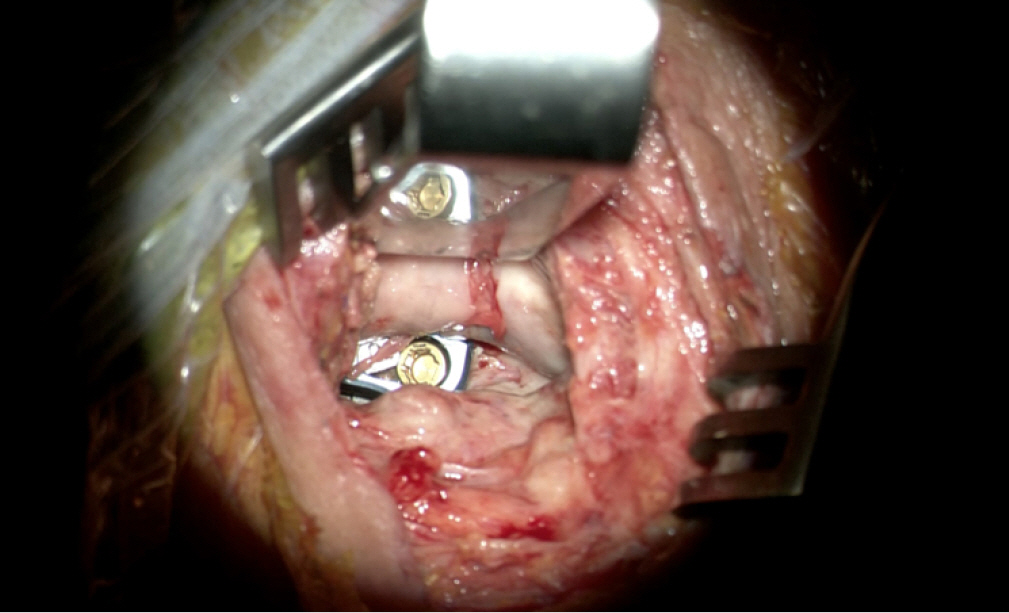
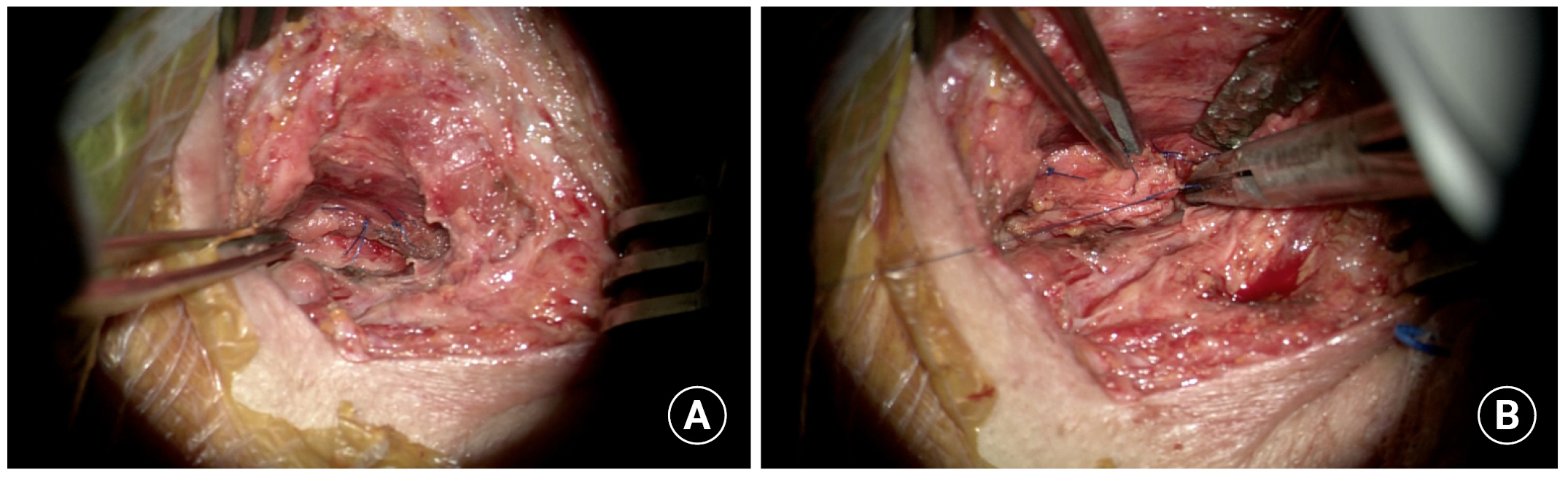
Suspicion arose that the cloudy fluid at the drain catheter removal site might have been orally ingested porridge rather than infectious pus, prompting consideration of pharyngeal wall perforation. This led to the decision to perform an emergent exploratory surgery. During the procedure, pharyngeal wall perforation was identified and repaired, with reinforcement provided using a sternocleidomastoid (SCM) muscle flap (Figs. 4 and 5). Following surgery, the patient was transferred to the neurosurgical intensive care unit (NSICU) for continued care. The intraoperative wound tissue culture yielded negative results. Subsequently, in consultation with the Infectious Disease team, the antibiotic regimen was adjusted to include piperacillin-tazobactam and vancomycin, which the patient continued to receive.
After the second surgery, minimal drainage was noted. The surgical site Jackson-Pratt (JP) drain was retained under negative pressure with the coordination of the Otolaryngology team. After a 12-day stay in the NSICU, the patient's pneumonia improved, enabling transfer to a general ward. Although two attempts at esophagography were made, the patient's limited cooperation rendered both efforts inconclusive. Given the minimal drainage and the clinical course, pharyngeal healing was hypothesized, prompting the initiation of oral feeding. Regrettably, this led to recurrent aspirations and a pneumonia relapse.
Consequently, L-tube feeding was instituted for approximately six weeks post-surgery, after which the patient successfully transitioned to an oral diet. Remarkably, no additional complications were encountered, such as surgical site infections or extensions to adjacent areas. Post-operative treatment was successfully concluded without further morbidity.
In this case, the patient's pharyngeal perforation was treated similarly to the few other cases reported in the literature. The treatment involved early surgical repair of the pharyngoesophageal perforation, supported by a sternocleidomastoid muscle flap. The wound was then closed over a vacuum drain. The decision for immediate follow-up surgery was based on the drainage of the oral diet through the JP drain, and other signs like fever, dysphagia, cough, and following aspiration pneumonia were critical in suspecting a pharyngeal perforation.
The patient developed a fever on the first day after surgery, and we initially judged this to be a physiologic fever. This is because most early post-operative fevers are caused by surgically stimulated inflammation and resolve spontaneously. However, post-operative fever rates at the surgical site are reportedly higher after posterior cervical spine surgery than after anterior cervical spine surgery3). That may have been the first clue that a pharyngeal perforation had occurred.
After surgery involving an anterior approach to the cervical spine, the most common complaint is dysphagia caused by pharyngoesophageal retraction. A more serious complication is the perforation of the pharyngeal or esophageal tissue. This perforation can lead to dysphagia, local soft-tissue infection, and deeper infection, which might result in hardware failure, pseudarthrosis, osteomyelitis/discitis, sepsis, and in severe cases, infectious mediastinitis and death4,5). The incidence of these complications ranges from 0.02% to 1.52% and is higher when the initial spinal injury is trauma-related2,4,6-9).
Acute injuries may occur accidentally during surgery due to incorrect placement or movement of sharp-toothed retractor blades in the esophagus. Retraction is especially dangerous when a nasogastric tube is used because the wall of the hypopharynx or esophagus might get "trapped" between the retractor and the tube. This can cause an ischemic injury and then a secondary perforation.8 Early detection and the proper treatment of pharyngoesophageal injury after anterior spinal surgery can improve the patient's chances by preventing further complications10).
The pharyngoesophageal junction is located posterior to the cricoid cartilage and is formed at the union between the pharynx and the esophagus. The region, Killian’s triangle (approximately at the level of C5-6), is known to be most vulnerable to mechanical injury as it lacks protective muscular layers11). Another frequently affected area in pharyngoesophageal injury is the lateral aspect of the thyrohyoid membrane (approximately at the level of C3-4)12). Esophageal injuries are more likely to occur at these two specific locations8).
When a patient has acute dysphagia after cervical spine surgery, physicians should consider the possibility of pharyngoesophageal perforation and immediately proceed with more diagnostic evaluations and treatment. The treatment depends on when the perforation is detected and how large it is. In the early stages, when the tissues are still healthy, the treatment of choice is primary suturing.2 This is made possible by checking for abnormalities in the drainage pattern during intensive post-operative care after anterior cervical spine surgery and by not overlooking the signs of dysphagia accompanied by fever.
This case highlights the critical need for prompt detection and intervention for pharyngeal perforation following ACDF, which is a rare yet severe complication. The perforation was effectively treated with rapid surgical repair using a sternocleidomastoid flap. Intensive post-operative care, paying close attention to signs such as abnormal drainage patterns at the surgical site and dysphagia accompanied by fever, is essential to prevent further complications and enhance the chances of a successful recovery.
NOTES
Ethics statement
The patient and guardian have consented to the submission of the case report for submission to the KJCCM.
Fig. 1.
The preoperative magnetic resonance imaging revealed severe stenosis with herniated nucleus pulposus at the C3-4 level, leading to cord compression and signal changes. This level was assessed as the symptomatic lesion, prompting the decision to proceed with anterior cervical discectomy and fusion surgery.

Fig. 2.
The image depicts the appearance after removing the drain tube, from which purulent, cloudy fluid was observed. External drainage continued even after the removal of the Jackson-Pratt drain. Since it was the first day post-surgery, the substance was assessed not as pus but as porridge the patient had orally ingested.

Fig. 3.
Due to decreased oxygen saturation and respiratory distress, immediate intubation was performed. Subsequent chest X-ray confirmed the presence of aspiration pneumonia.

REFERENCES
1. Lee S, Cho DC, Chon H, Roh SW, Choi I, Park JH. Comparison between anterior cervical decompression with fusion and posterior cervical fusion with wide facetectomy for treatment of severe bony foraminal stenosis. J Korean Neurosurg Soc 2021;64:552–561.




2. Vrouenraets BC, Been HD, Brouwer-Mladin R, Bruno M, van Lanschot JJ. Esophageal perforation associated with cervical spine surgery: report of two cases and review of the literature. Dig Surg 2004;21:246–249.



3. Lee S, Jung SK, Kim HB, Roh SW, Jeon SR, Park JH. Postoperative non-pathological fever following posterior cervical fusion surgery: Is laminoplasty a better preventive method than laminectomy? J Korean Neurosurg Soc 2020;63:487–494.




4. et al. Esophageal perforation after anterior cervical spine surgery: a systematic review of the literature. J Neurosurg Spine 2016;25:285–291.


5. van Berge Henegouwen DP, Roukema JA, de Nie JC, vd Werken C. Esophageal perforation during surgery on the cervical spine. Neurosurgery 1991;29:766–768.



6. Ji H, Liu D, You W, Zhou F, Liu Z. Success in esophageal perforation repair with open-wound management after revision cervical spine surgery: a case report. Spine (Phila Pa 1976) 2015;40:E183–185.

7. Benazzo M, Spasiano R, Bertino G, Occhini A, Gatti P. Sternocleidomastoid muscle flap in esophageal perforation repair after cervical spine surgery: concepts, techniques, and personal experience. J Spinal Disord Tech 2008;21:597–605.

8. Orlando ER, Caroli E, Ferrante L. Management of the cervical esophagus and hypofarinx perforations complicating anterior cervical spine surgery. Spine (Phila Pa 1976) 2003;28:E290–E295.


9. Ahn SH, Lee SH, Kim ES, Eoh W. Successful repair of esophageal perforation after anterior cervical fusion for cervical spine fracture. J Clin Neurosci 2011;18:1374–1380.


10. Park JS, Kim YB, Hong HJ, Hwang SN. Esophageal Injury Following Anterior Cervical Plate Fixation. J Korean Neurosurg Soc 2005;37:141–145.
- TOOLS