Utility of Hemolung® in Acute Neurological Crisis with Ventilatory Failure
Article information
Extracorporeal carbon dioxide removal (ECCO2R) is a process where filtration of CO2 happens with the blood flow, a central filter, a pump, and an exchange of air/Oxygen mixture. The flow of the gas mixture decides the percentage removal of CO2. The late last century saw marked improvement in the technology, although initial efforts were flawed with the large size of the equipment, complications, and no major impact on the outcome. Recently FDA approved technology for ECCO2R from ALung® i.e Hemolung® device which was incorporated in the last decade. The key utility is mainly in patients with severe COPD with acute respiratory failure. Acute respiratory with a pulmonary complication like ARDS or edema requires reduction of driving pressure by keeping the tidal volume low and higher PEEP. This commonly leads to an increased level of partial pressure of CO2, hence direct impact to abnormal brain hemodynamics with acute brain injury1). Here we suggest early use of Hemolung® in such a situation.
Early use of ECCO2R can be used in COPD acute respiratory to avoid intubation. Most of these patients have bi-level positive pressure ventilation attempted before proceeding to intubation. There is evidence for the avoidance of invasive ventilation with intubation with early application of ECCO2R2-7). Retention of CO2 and anticipatory reduction in PH are commonly seen during the protected lung strategy in ARDS care. ECCO2R can be used to reduce the build of CO28). With an established pandemic of SARS-CoV2 and extensive ARDS care in the intensive care units, the need for ECCO2R is more obvious 9,10).
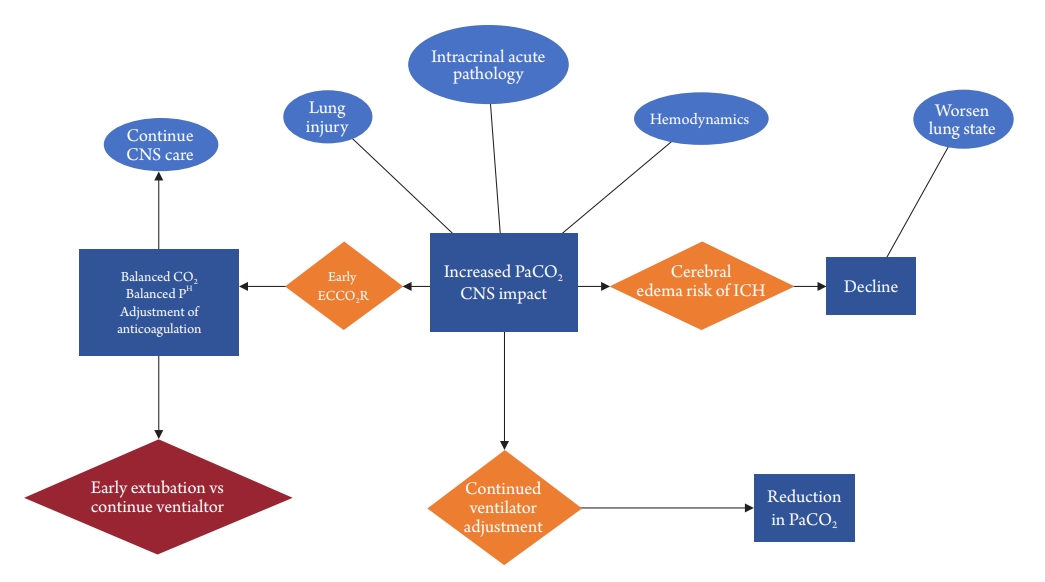
Cerebral hemodynamic is directly impacted by the arterial partial pressure of CO2 and O2. The impact of CO2 is steeper and more obvious. The oxygenation can be maintained with a higher range if adequate circulation is present. Acute respiratory failure with ARDS in acute neurological injury is commonly seen in the neurocritical care practice. There is a constant struggle to protect the lung from ventilatory-induced lung injury and the impact of rising CO2 on the injured brain (Fig. 1). The utility of ECCO2R can be a help. A lower dose of anticoagulation infusion can be used to avoid any further hemorrhage in an active condition of intracranial hemorrhage11). Hemolung® uses room airflow to remove CO2 without a need for a high flow oxygen supply. This device will be useful in conditions as mentioned with acute brain injury.
In conclusion, we suggest that Hemolung® device should be present in high capacity neurocritical care unit. Neurointensivist training and competency need to be maintained. Early inclusion of this device may be required where a lung-protective approach is used especially in ARDS patients. Further case series and prospective observational trials will probably show that this technology is useful.
Notes
Conflict of interest
No potential conflict of interest relevant to this article was reported.