Analysis of Nitrogen Balance Test in Patients With Traumatic Brain Injury
Article information
Abstract
Background
This study aimed to analyze the catabolic phases of patients with traumatic brain injury (TBI) by performing the Nitrogen Balance Test (NB Test).
Methods
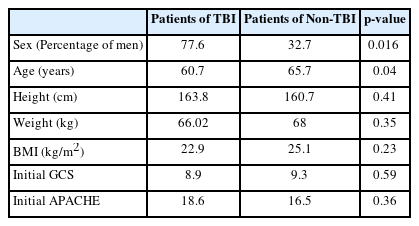
This single-centered, retrospective study included data from 292 patients who underwent NB tests from 2019 to 2022 and categorized them as TBI and Non-TBI groups. The basic clinical factors (gender, age, and initial GCS), critical care factors (APACHE, SOFA, and ICU stay days), and outcomes (GOS). The trend of the NB test was investigated in all groups and analyzed the statistical correlation of the NB test was with severity, critical care factors, and outcomes.
Results
A total of 52 patients were found to have TBI. The 26 out of 52 TBI patients underwent the second NB test 1 week after the first NB test. The deficiency of protein calculated was 24.375 g. There was a significant statistical difference of NB test patterns between the non-TBI and TBI patients.
Conclusion
Physicians should be aware of the catabolic phases of acute TBI events indicating notable protein loss in the patients. Therefore, we should consider the additional supply of protein when managing TBI patients.
INTRODUCTION
Many patients fall into the catabolic phase in intensive care units1-2). In critically ill patients, stress hormones and inflammatory mediators are activated, and metabolically, proteolysis by catabolic action occurs. Especially, in stressful situation such as post trauma status, more reactions are induced by stress, ultimately leading to catabolic effects. The main metabolic change in response to injury that leads to a series of reactions is the reduction of the normal anabolic effect of insulin. After trauma, free fatty acids and triglycerides are consumed such as primary sources of energy. At the same time, proteolysis leads the negative nitrogen balance. When this catabolic phase is severe, many patients tend to have a poor prognosis3-9). This trend applies to critically ill and neurological critically ill patients10). Neurological critically ill patients also have higher morbidity and mortality if insufficient nutrient supply is poor11-13). So, proper nutrition supply in the catabolic phase such as early enteral nutrition at a proper time is very important. Despite the importance of the catabolic phase, there are only a few studies on catabolic trends neurotrauma patients exhibit over time after injury. There are many tests that can determine the degree of catabolic phase, but in practice, the nitrogen balance test (NB test) is the most commonly used14-23). So we investigated the trends of catabolic phase in head trauma patients and the difference from other neurologically critical patients by using NB test.
MATERIALS AND METHODS
Study population and protocol
This study included patients expected to be admitted to the neurological intensive care unit (NCU) for >1 week from June 2019 to March 2021. In principle, the treatment protocol of the intensive care unit of this hospital is to perform the NB test once a week. However, NB tests were not performed for patients with renal failure, those who started eating by mouth instead of L tube and found it difficult to calculate intake, those whose caregivers refused active treatment, and those who were abruptly discharged or transferred to general hospital rooms.
Study design
All patients were classified into two groups: trauma and non-trauma (Tumor and stroke). Basic clinical factors, such as age, sex, mortality, height, weight, BMI, and other factors were examined in all patient groups. Additionally, initial GCS, initial Apache score, NCU check-in period, SOFA score, NB test results (at the time of admission, 1-week later, and 2-weeks later) and the GOS at 3 months later were investigated.
We then first analyzed whether there was a significant change in the trend of the NB test statistically. We then analyzed the NB test, trauma, initial GCS, initial Apache score, NCU admission period, SOFA score, and GOS at 3 months later.
Statiscal analysis
Statistical analysis was performed using SPSS Statistics 25.0 (IBM, Chicago, USA). Fisher exact tests or χ2 tests were performed for categorical variables, while independent t-test for continuous variables of clinical factors. A p-value <0.05 was considered statistically significant. All data are presented as mean ± standard deviation for continuous variables.
RESULTS
Baseline characteristics
A total of 3,768 patients were admitted to the NCU during the study period. Among these neuro-surgical patients, 292 neuro-critically ill patients were included in the final analysis. Among the 292 patients, the number of TBI patients was 52. Among the 240 non-trauma patients, 105 had brain tumor-related diseases, 111 had stroke, and 24 had other diseases, such as seizure, wound infection, and sepsis. The proportion of men in trauma patients was higher than that in non-trauma patients, and the proportion of younger age in trauma patients was higher than that in non-trauma patients statistically. The initial GC and APACHE scores reflecting severity did not show a statistically significant difference (Table 1).
Trend of nitrogen balance test
Of the 292 patients, 160 completed the second NB test and 79 completed the third NB test. Analysis of NB test trends in all group shows -6.77 ± 4.9 g/d in the first NB test, -7.24 ± 5.1 g/d in the second NB test, and -4.3 ± 5.3 g/d at 2 weeks follow-up. This study found that the NB test did not improve until >2 weeks after admission to the NCU (Fig. 1). Next, the authors analyzed NB test trends by dividing them into traumatic and non-traumatic groups (Fig. 2). The first NB test was -7.1 g/d in the trauma group and -7.3 g/d in the non-traumatic group, with no statistical difference. However, in the second NB test, there was a statistical difference in the NB test results of the non-traumatic and traumatic groups. In the non-traumatic group, the second NB test value was –7.2 g/d, which was not significantly changed compared to first NB test, but in the trauma group, the second NB was -11.2 g/d, which was significantly lower than 1st NB (p = 0.005) (Fig. 2). In the third NB test, the traumatic and non-traumatic groups showed a slight deviation from the catabolic phase with -4.7 g/d -4.2 g/d, respectively.
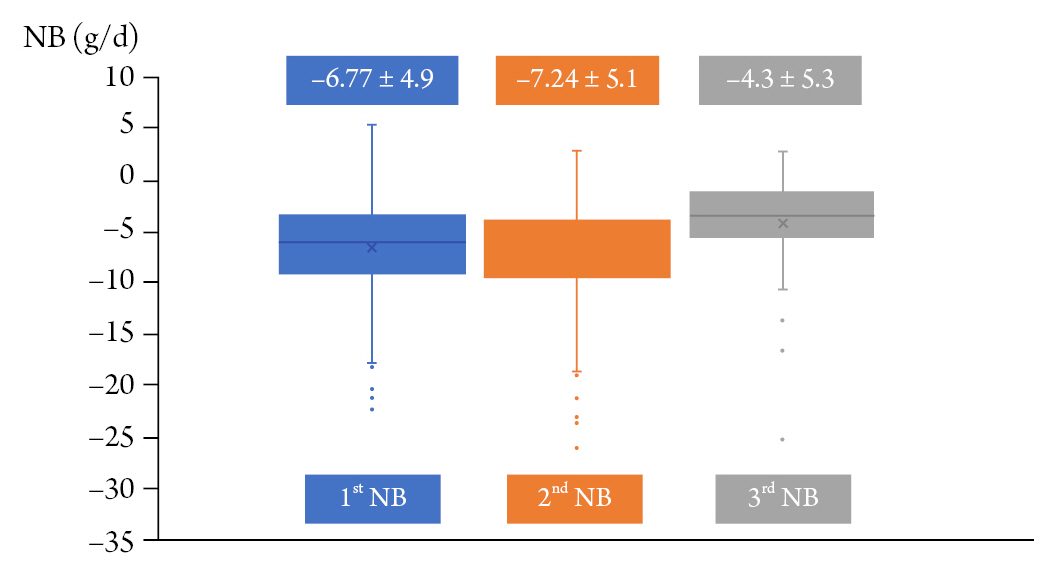
Trends of nitrogen balance test (NB test) in all participants. The initial NB tests revealed the catabolic phase of the patients. And it sustained until the 2nd NB test. The catabolic phase was recovered at 3rd NB tests, it was performed at 2weeks later.
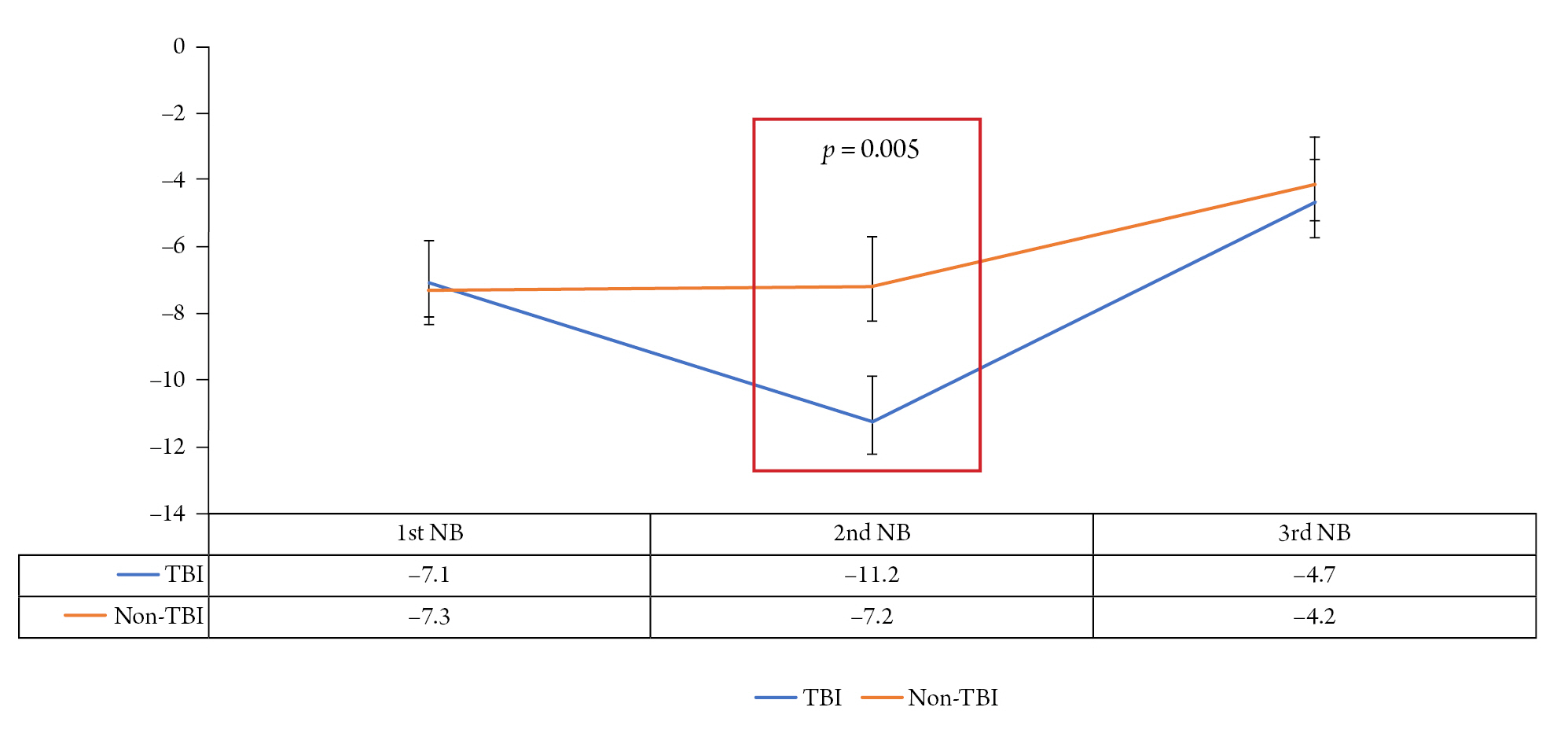
Nitrogen balance test (NB test) results according to the presence of trauma. In the TBI groups, 2nd NB test was revealed that the catabolic phase was worsened. In contrast, in the non-traumatic group, the 2nd NB test did not differ significantly from the 1st NB test. Both 3rd NB tests showed improvement in the catabolic phase.
Analysis of the second NB tests in TBI group
We analyzed the input and output of the second NB test to determine the causes of increased negative NB tests in the trauma group (Fig. 3). As a result, even though the input increased from 8.06 to 11.07, the NB test value became more negative because the output increased a lot. Thus, it can be seen why the second NB test in TBI group value became more negative was not because of decreased input, but because of increased output.
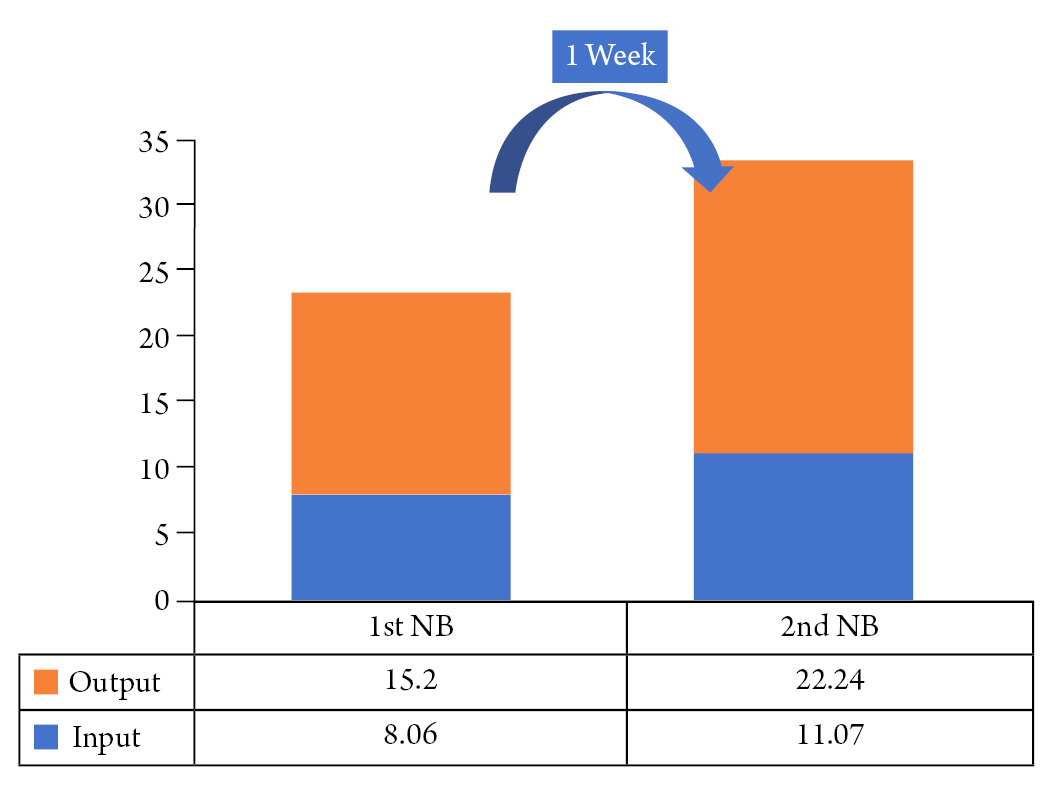
Analysis of first and second nitrogen balance test (NB test) in TBI group, focused on the input and output. Compared to the time of the first NB trial, it can be seen that the diet supply in patients has increased. However, even though the input increased, the output increase was much higher, and the overall negative was worse in the second NB test. However, it can be seen that the cause of the second NB test in TBI group is not because intput is reduced, but because output is increased.
Correlation between NB test and severity and outcome factors
We also analyzed the correlation between NB test and severity and outcome factors. Severity was evaluated as the initial GCS, SOFA, and APACHE score, and the outcome was evaluated as ICU tenure and GOS at 3 months later. As a result, our NB test did not demonstrate a statistical correlation between severity and outcome (Table 2).
DISCUSSION
This study divided the NCU patients into traumatic and non-traumatic groups to investigate trends in NB tests. The results showed that the catabolic phase was increased on the second NB test, that is, the NB test 1 week after the trauma, in the head trauma patient group. It was not until 2 weeks later that we observed improved catabolic phase. The catabolic phase in ICU patients has already been reported in many prior studies24-28). The most reliable test for determining at this catabolic phase may be the NB test24,29-35).
This study analyzed the worsening of the second NB test in patients with TBI. As a result, it was confirmed that the NB test worsened due to an increase in protein output, rather than a decrease in the input or nutrition supply. This worsening of the catabolic phase on the NB test of the second phase can have various causes. For examples, sedation, targeted temperature management, and multiple operations can worse the catabolic phase. When coma therapy or body temperature is lowered, caloric requirements tend to decrease36). In patients with unstable vital signs, nutrition may not be absorbed in the intestine even if it is supplied. We performed coma therapy and target temperature management for ICP control in patients with severe brain injury. About 1 week after admission, this treatment should end; thus, the NB test may appear as the catabolic phase. Therefore, further study should be conducted for correcting surgical and intensive care factors.
This study should be of interest because the nutrition-related data was carefully collected because it was a protocol base study, which was consistent with treatment protocols because it was conducted in a single institution, and through multidisciplinary rounds. In addition, nutrition-related data was measured daily by a clinical dietitian during multidisciplinary rounds, and other SOFA and Apache scores were automatically measured. However, further large, prospective studies with surgical factor correction and multiple intensive care factor corrections should be conducted in the future.
This study had limitations. First, there were high dropout rates. Second, this was a single-centered study with few participants. Third, this was retrospective study. The 292 of of 3,700 patients, or <10 %, have been introduced, which is likely to result in the omission of very severe cases. In particular, due to the law of discontinuation of life-sustaining treatment, there is a tendency to miss a lot of serious illness because caregivers give up treatment early. Finally, many patients tend to be missing when renal function declined because it was an NB test study. Thus, there may also be cases where the catabolic phase was clearly present but were missing.
CONCLUSION
For many critically-ill patients, especially the head trauma group, the NB test accurately showed more severe catabolic phase than the non-traumatic group. Therefore, actively managing the catabolic phase by attempting to improve the NB test through protein supply from the beginning should be practiced in head trauma patients.
Notes
Conflict of interest
There is no conflict of interest to disclose.