 |
 |
- Search
| J Neurointensive Care > Volume 6(1); 2023 > Article |
|
Abstract
Neurocritical care has emerged as a specialized field addressing the complex needs of patients with acute neurological disorders, such as stroke, brain tumor and traumatic brain injury. The clinical management of these patients necessitates precise, individualized nutritional support due to the significant variability in neurological deficits and resting energy expenditure (REE) based on factors including stroke phase, type (hemorrhagic or ischemic), and intracranial pressure and activity of neuronal cells. This emphasizes the need for accurate, patient-specific nutritional recommendations, achievable through indirect calorimetry. Traditional predictive equations may not accurately capture the diverse nutritional requirements of neurocritical patients. Indirect calorimetry offers a more reliable, personalized approach to determining patients' nutritional needs, crucial for this heterogeneous population. Furthermore, clinical practice often inadequately addresses nutritional needs in neurocritical patients, highlighting the importance of optimizing nutritional support to enhance patient outcomes. Indirect calorimetry also plays a critical role in assessing patients with non-normal body temperatures. Hypothermia affects the body's metabolic rate and overall energy expenditure, making it challenging to evaluate energy requirements during hypothermia treatment. Indirect calorimetry can provide more accurate assessments under such conditions. In conclusion, employing indirect calorimetry in neurocritical care is essential for accurate, individualized nutritional support. By accounting for factors such as stroke type, location, intracranial pressure and body temperature, indirect calorimetry offers valuable insights and improved patient care, emphasizing its indispensability in managing neurocritical patients.
Neurocritical care has evolved as a specialized field that aims to address the complex needs of patients with acute neurological disorders, including stroke, brain tumor, traumatic brain injury, and increased intracranial pressure. The clinical management of such patients requires precise and individualized nutritional support, as neurological vulnerability, and resting energy expenditure (REE) vary greatly depending on factors such as the stroke phase, type (hemorrhagic or ischemic), and intracranial pressure. This highlights the need for accurate and patient-specific nutritional recommendations, which can be provided with indirect calorimetry.
Traditional predictive equations may not accurately reflect the heterogeneous nutritional requirements of patients in neurocritical care. A 2021 ASPEN study demonstrated inconsistent nutritional guidelines for acute ischemic stroke patients (25 kcal/kg) and acute hemorrhagic stroke patients (30 kcal/kg)1). Indirect calorimetry has been shown to provide a more reliable and personalized approach to determining patients' nutritional needs, which is crucial in this diverse patient population2,3).
Moreover, clinical practice often falls short in providing adequate nutrition for neurocritical patients. A 2022 ASPEN study found that only 48% of the caloric requirements measured by indirect calorimetry were provided within the first 72 hours, although this figure improved to 87% by day 74). This underlines the importance of optimizing nutritional support to improve patient outcomes.
Indirect calorimetry also plays a vital role in evaluating patients with abnormal body temperatures. Hypothermia, for example, affects the body's metabolic rate and overall energy expenditure5). Assessing energy requirements during hypothermia treatment is challenging, as some studies have reported acute hypermetabolism in severe traumatic brain injury patients with energy requirements up to 200% higher than expected. Indirect calorimetry can help provide more accurate assessments of energy requirements under such conditions6,7). Collectively, the use of indirect calorimetry in neurocritical care is essential to ensure accurate, individualized nutritional support. By considering factors such as stroke type, location, and body temperature, indirect calorimetry offers valuable insights and improved patient care, emphasizing its necessity in the management of neurocritical patients.
In this review, we emphasize the importance of measuring basal metabolic rate (BMR) using calorimeters in neuro-critical care. Direct calorimeters, which directly measure heat from an individual in a closed system, are not used clinically. Instead, indirect calorimeters (IC) are employed, especially for patients on ventilators or with sepsis, who require measurements at least once a week (Fig. 1). IC is employed to estimate energy requirements for mechanically ventilated or septic patients by calculating the ratio of oxygen consumption and carbon dioxide production during respiration2,3). If measurement is not possible, existing formulas should be used or nitrogen equilibrium should be calculated. IC is particularly crucial in situations where BMR calculation is challenging, such as acute/chronic respiratory failure syndrome, large open wounds or burns, malnutrition with altered body composition, multiple/neurological trauma, multiple organ failure, organ transplantation, sepsis, systemic inflammatory response syndrome, and the use of muscle relaxants or barbiturates. IC helps accurately calculate resting energy expenditure (REE) to reduce metabolic and respiratory complications in severe illness including neuro-critical crisis. When using IC, certain concerns should be considered, such as adding 5% of calories for thermogenesis in fasting measurements for patients on intermittent nutrition and using the measured REE at 100% without an activity index for ICU patients. Overall, indirect calorimetry plays a vital role in neuro-critical care by providing accurate BMR measurements and individualized therapy for critically ill patients (Table 1)2,3).
In clinical settings, accurately assessing a patient's BMR is essential for informed decision-making regarding their care. Indirect calorimetry is a valuable method used for this purpose. To ensure the precision of the measurements, neurointensivists must take several factors into account and follow a specific process.
Before the measurement begins, the patient needs to have rested for at least 30 minutes. If the patient is experiencing pain or discomfort, administering analgesics or sedatives may be necessary. After any painful procedures, a minimum waiting time of 1 hour is recommended. It is also important to minimize nursing activities before the measurement to avoid interference.
When using indirect calorimetry to measure BMR, neurointensivists must consider the clinical environment's influence. Nutrition is one such aspect. In cases of continuous feeding, the feeding rate and formula should remain unchanged for at least 12 hours before the measurement. For intermittent feeding, a 1-hour wait is required after feeding if the measurement includes the thermic effect of food, while a 4-hour wait is necessary if excluding it.
Mechanical ventilation is another critical factor. Throughout the measurement period, ventilation should remain unchanged. After adjusting ventilator settings, a 90-minute waiting time is required. It is also crucial to ensure that there are no leaks in the system.
For patients undergoing blood dialysis, BMR measurements should be taken 3-4 hours after the procedure.
The required equipment for the process includes cables, a water trap, and a circuit. To perform the measurement, first, prepare the circuit for connecting to the IC module. Next, connect the circuit and water trap to the IC module. Remove the existing monitor module and connect the IC module. Attach the opposite end of the spirometry kit to the endotracheal tube. Finally, start the measurement software, such as the OhmedaCom research tool. Allow approximately 5 minutes for calibration, then wait for 15-20 minutes for stable data collection in the "steady-state" condition.
1) Pre-measurement preparation:
• Ensure the patient has rested for at least 30 minutes before the measurement.
• Administer analgesics or sedatives if necessary.
• Measure BMR at least 1 hour after any painful procedure.
• Minimize nursing activities before the measurement.
2) Factors to consider during BMR measurement:
(a) Nutrition
• Continuous feeding: Maintain a constant feeding rate and formula for at least 12 hours before measurement.
• Intermittent feeding: If measuring BMR including the thermic effect of food, wait for 1 hour after feeding. If excluding the thermic effect of food, wait for 4 hours after feeding.
(b) Mechanical ventilation:
• Ensure no changes in ventilation occur during the measurement period.
• Wait for at least 90 minutes after any adjustments to the ventilator settings.
• Ensure there are no leaks in the system.
(c) Dialysis:
• Measure BMR 3-4 hours after blood dialysis.
3) Required equipment: Cables, water trap, and circuit.
4) Measurement process (Fig. 2)
IC measures energy expenditure by analyzing respiratory gases (O2 consumption and CO2 production) and calculates basal metabolic rate using the modified Weir equation:
REE (Kcal/day) = 1.44 × (VO2 (ml/min) × 3.94) + [VCO2 (ml/min) × 1.11])
During IC measurements, the respiratory quotient (RQ) is calculated using VO2 and VCO2, serving as an indicator of substrate utilization. In other words, RQ evaluates the ratio of consumed oxygen to expelled carbon dioxide to determine the primary energy source being used.
RQ = VCO2/VO2
The three primary energy sources (fat, protein, and carbohydrates) each generate energy and expel carbon dioxide in the body by consuming oxygen, with different oxygen and carbon dioxide ratios. This is the basis of indirect calorimetry. The physiological range of the respiratory quotient (RQ) is 0.67 - 1.3, with an approximate RQ of 0.8 for a mixed oral diet. An RQ value below 0.7 suggests nutritional deficiency, with fat being the primary energy source (Table 2).
If the measured RQ value does not reach 0.8 despite providing calories based on the measured REE, calorie intake can be increased up to 1.2-1.5 times the REE. RQ values below 0.67 or above 1.3 indicate measurement errors and necessitate re-measurement. If the coefficient of variation is not less than 10%, wait for some time and recheck the measurement values.
• An RQ of 1.0 indicates that carbohydrates are the primary fuel source, as one molecule of carbon dioxide is produced for each molecule of oxygen consumed during carbohydrate metabolism.
• An RQ of 0.7 suggests that fats are the main energy source, as fewer carbon dioxide molecules are produced per molecule of oxygen consumed during fat metabolism.
• An RQ between 0.7 and 1.0 implies a mix of carbohydrates and fats are being used for energy production.
IC, which measures VO2 and VCO2, represents real-time energy metabolism8). Although the evidence level is low, international nutritional guidelines for adult critically ill patients recommend evaluating REE using indirect calorimetry (Grade B recommendation)9). IC measurement is not a life-saving purpose, but rather a monitoring tool providing information on metabolism. A retrospective study on acutely ill patients showed a U-shaped association between initial nutritional intake and 60-day mortality, emphasizing the clinical risk of overfeeding and underfeeding and the need for individual energy requirements measurement10). A 2020 systematic review and meta-analysis found that, although good results were not confirmed when providing nutrition based on IC measurements, the IC measurement patient group met the target energy more accurately than the patient group receiving nutrition through predictive equations11). A separate meta-analysis conducted in Europe in 2021 found a 23% reduction in short-term mortality when patient energy intake targets were assessed using IC12). Most meta-analyses did not prove shorter ICU stays or mechanical ventilation durations in patient groups receiving nutrition based on IC, likely due to higher CO2 production resulting from higher caloric intake, which potentially extended ICU stays and mechanical ventilation durations1).
Indirect calorimetry measurements should not be performed in certain clinical situations due to the potential for inaccurate results. These contraindications include:
① High levels of inspired oxygen (FiO2 ≥ 60).
② Elevated positive end-expiratory pressure (PEEP ≥ 12 cm H2O).
③ Patients experiencing hyper- or hypoventilation, as irregular breathing patterns can lead to inaccurate tidal volume measurements.
④ The presence of a leak, such as from a chest tube or bronchopleural fistula, which can limit the collection of all expired gas samples.
⑤ Moisture in the measurement system.
⑥ Patients who have undergone dialysis on the same day and have experienced significant volume loss.
⑦ Patients with severe irritability, as this can interfere with the measurement process.
IC has several advantages and disadvantages assessing the energy needs of critically ill patients. On the positive side, IC-based nutrition therapy has the potential to improve patient outcomes compared to predictive equation-based methods. IC is considered the gold standard for measuring resting energy expenditure (REE) in various international guidelines and allows for personalized nutrition therapy during the acute phase of critical illness.
However, there are some downsides to consider. IC devices are unable to measure non-nutritional calories, and there is a risk of refeeding syndrome, a clinical complication that can occur due to fluid and electrolyte shifts during aggressive nutritional support in malnourished patients. Additionally, cost, time, and human resource requirements may pose challenges when implementing IC in critical care.
There are also specific limitations to using IC in clinical situations. The accuracy of VO2 and VCO2 measurements can be compromised in patients with high oxygen requirements (FiO2 > 0.7), elevated positive end-expiratory pressure (PEEP > 12 cmH20), or air leaks (e.g., pneumothorax, emphysema, tracheoesophageal fistula). Assessments may be imprecise for patients using nebulization or wet sensors, and evaluations can be difficult for those using non-invasive ventilation (NIV) or high-flow nasal oxygen (HFNO). Finally, IC is not applicable for patients receiving non-mechanical oxygen therapy (Table 3).
IC has several implications for neurocritical care patients, as neurological deficits and REE can vary greatly depending on stroke stage, type (hemorrhagic or ischemic), location and intracranial pressure. This highlights the individualized nature of nutritional requirements in these patients.
According to a 2021 ASPEN study, appropriate nutrition guidelines for acute ischemic stroke patients are 25 kcal/kg, while for acute hemorrhagic stroke patients, they are 30 kcal/kg13). These inconsistent nutritional requirements can be better addressed by using IC compared to predictive equations, providing patients with optimized nutrition. A 2022 ASPEN study involving acute brain injury patients showed that during the first 72 hours, only 48% of the calorie requirements measured by IC were provided (although it is recommended to reach >80% of the target), but by day 7, 87% of the target was achieved4). This suggests that in clinical settings, patients are often provided with less nutrition than they actually require.
In hypothermic conditions, that is condition of targeted therapeutic hypothermia, metabolic rates and overall energy consumption are reduced. IC is a valuable tool to assess these changes, as there are limited alternative clinical assessment methods. Research on acute ischemic stroke patients maintaining hypothermia (33°C) showed a 30% decrease in energy requirements during the first 24-72 hours compared to normothermic patients14). However, some studies on severe traumatic brain injury patients observed excessive hypermetabolism during the acute phase, with energy requirements up to 200% higher than predicted. This makes evaluating energy requirements in these patients difficult when combined with hypothermic treatment.
In a 2021, RCT study involving severe traumatic brain injury patients, those receiving preventive hypothermic treatment (33-35°C) had approximately 20% lower energy requirements measured by IC compared to normothermic patients, which persisted until rewarming15). Acute normothermic patients exhibited a hypermetabolic state. After two weeks, when hypothermic patients were rewarmed to normal temperature, they also exhibited a hypermetabolic state similar to normothermic patients.
A 2015 retrospective Japanese study on stroke patients found that subacute patients did not exhibit hypermetabolism, and their stress factors were measured at 1.0-1.1. This underlines the variability in metabolic states and nutritional requirements among different types of neurocritical care patients, further highlighting the importance of using IC for individualized assessments16).
Indirect calorimetry is particularly useful in neurocritical care due to the heterogeneous nutritional requirements of patients with acute neuro-critical disease and increased intracranial pressure. Studies have shown inconsistent nutritional guidelines for patients with acute ischemic stroke (25 kcal/kg) and acute hemorrhagic stroke (30 kcal/kg), indicating the need for a more personalized approach. Indirect calorimetry can help optimize nutrition for these patients compared to using predictive equations. Furthermore, it has been demonstrated that clinical practice often underdelivers compared to actual nutritional requirements, highlighting the importance of using indirect calorimetry to improve patient outcomes.
In conclusion, indirect calorimetry is a valuable tool in neurocritical care, providing accurate and individualized nutritional support for patients with acute neurological disorders. Its use can improve patient outcomes and optimize management, emphasizing its essential role in the care of neurocritical patients.
Fig. 1.
Comparison of direct and indirect calorimeters. Representation illustrating the differences between direct and indirect calorimeters.
This figure provides a side-by-side comparison of direct and indirect calorimeters, showcasing their distinct features and methodologies. It visually highlights the key differences in measuring energy expenditure: direct calorimetry captures heat production through a calorimeter chamber, while indirect calorimetry estimates metabolic rate by analyzing respiratory gas exchange. The figure aims to elucidate the unique aspects of each method, offering a clear understanding of their respective approaches to assessing energy expenditure.

Fig. 2.
Indirect calorimetry measurement process.
This figure provides a visual narrative of the essential steps in the indirect calorimetry measurement process for assessing basal metabolic rate in a clinical setting. The illustration guides the viewer through the preparation and connection of the circuit to the indirect calorimetry module, the integration of the water trap, the removal and attachment of monitor modules, the connection between the spirometry kit and endotracheal tube, and finally, the initiation and calibration of the measurement software.
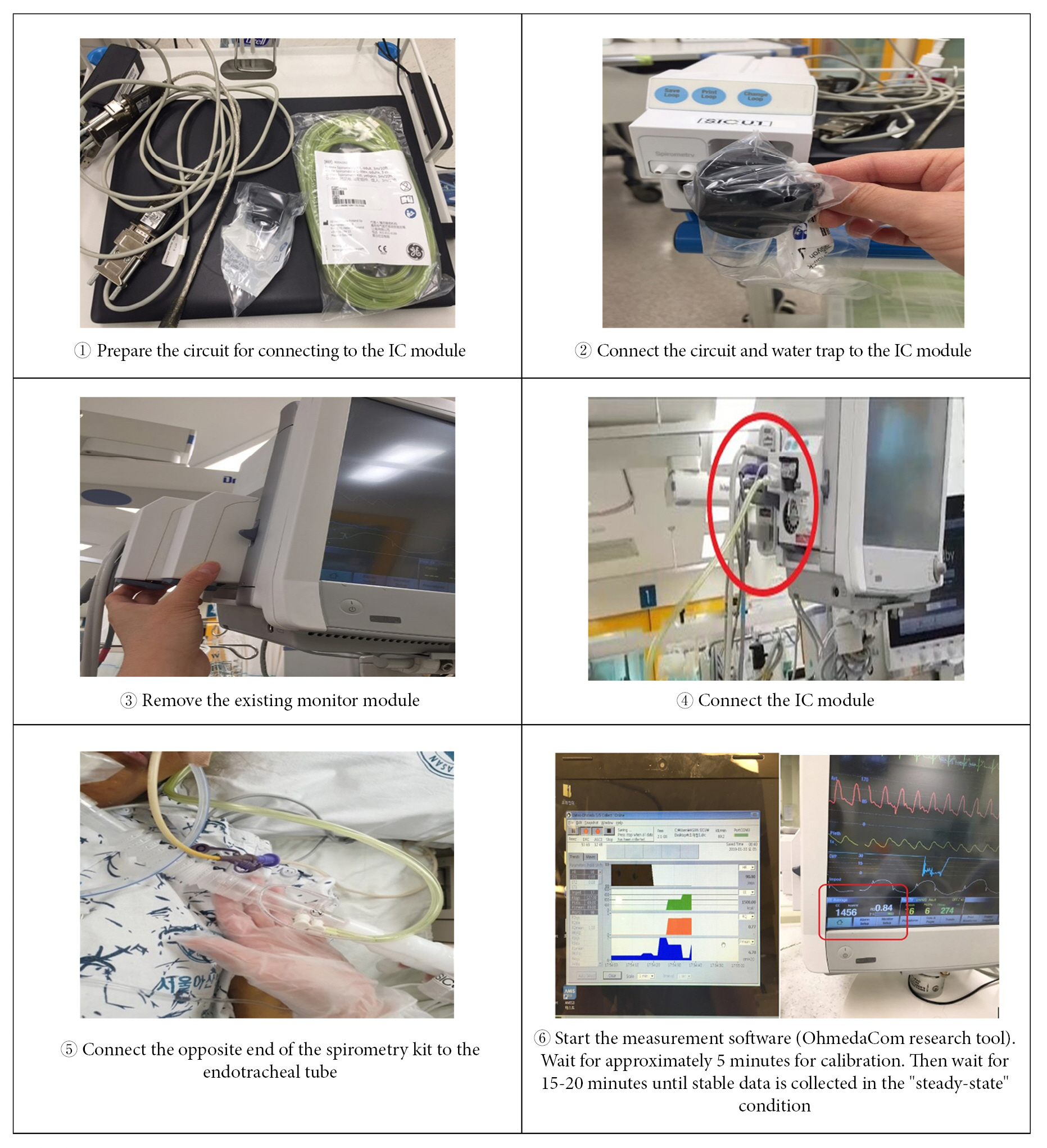
Table 1.
Assessing energy requirements in neurocritical care:indications and considerations for basal metabolic rate calculation and indirect calorimetry
Table 2.
Source of energy and respiratory quotient used for basal metabolism
| Substrates | VO2 | VCO2 | RQ | Kcal/g |
|---|---|---|---|---|
| Lipid | 2.0 | 1.4 | 0.7 | 9.1 |
| Protein | 0.96 | 0.78 | 0.82 | 4.0 |
| Carbohydrate | 0.74 | 0.74 | 1.0 | 3.7 |
| Mixed feeding | 0.85 | |||
| Overfeeding | 1.1-1.2 |
Table 3.
Pros and cons of indirect calorimetry
REFERENCES
1. De Waele E, van Zanten AR. Routine use of indirect calorimetry in critically ill patients: Pros and cons. Critical Care 2022;26:123.


2. Holdy KE. Monitoring energy metabolism with indirect calorimetry: instruments, interpretation, and clinical application. Nutr Clin Pract 2004;19:447–454.


3. Wooley JA, Sax HC. Indirect calorimetry: applications to practice. Nutr Clin Pract 2003;18:434–439.


4. May CC, Harris EA, Hannawi Y, Smetana KS. Evaluation of energy intake compared with indirect calorimetry requirements in critically ill patients with acute brain injury. JPEN J Parenter Enteral Nutr 2022;46:1176–1182.



5. Hills AP, Mokhtar N, Byrne NM. Assessment of physical activity and energy expenditure: an overview of objective measures. Front Nutr 2014;1:5.



6. McClave SA, Spain DA, Skolnick JL, Lowen CC, Kieber MJ, Wickerham PS, et al. Achievement of steady state optimizes results when performing indirect calorimetry. JPEN J Parenter Enteral Nutr 2003;27:16–20.


7. Reeves MM, Capra S. Predicting energy requirements in the clinical setting: are current methods evidence based? Nutr Rev 2003;61:143–151.


8. Moonen HP, Beckers KJ, van Zanten AR. Energy expenditure and indirect calorimetry in critical illness and convalescence: current evidence and practical considerations. J Intensive Care 2021;9:8.




9. Singer P, Blaser AR, Berger MM, Alhazzani W, Calder PC, Casaer MP, et al. ESPEN guideline on clinical nutrition in the intensive care unit. Clin Nutr 2019;38:48–79.


10. Zusman O, Theilla M, Cohen J, Kagan I, Bendavid I, Singer P. Resting energy expenditure, calorie and protein consumption in critically ill patients: a retrospective cohort study. Crit Care 2016;20:367.




11. Tatucu-Babet OA, Fetterplace K, Lambell K, Miller E, Deane AM, Ridley EJ. Is energy delivery guided by indirect calorimetry associated with improved clinical outcomes in critically Ill patients? A systematic review and meta-analysis. Nutr Metab Insights 2020;13:1178638820903295.




12. Duan JY, Zheng WH, Zhou H, Xu Y, Huang HB. Energy delivery guided by indirect calorimetry in critically ill patients: a systematic review and meta-analysis. Crit Care 2021;25:88.




13. Smetana KS, Hannawi Y, May CC. Indirect calorimetry measurements compared with guideline weight-based energy calculations in critically Ill stroke patients. JPEN J Parenter Enteral Nutr 2021;45:1484–1490.



14. Bardutzky J, Georgiadis D, Kollmar R, Schwab S. Energy expenditure in ischemic stroke patients treated with moderate hypothermia. Intensive Care Med 2004;30:151–154.



- TOOLS






