Comparison Between Complications of Pentothal Coma Therapy and Targeted Temperature Management in Traumatic Brain Injury Patients
Article information
Abstract
Background
Pentothal coma therapy (PCT) and targeted temperature management (TTM) are considered the most aggressive medical care for patients with severe traumatic brain injury (TBI). However, there is very little comparison between these two options. We compared the survival rates and complications between the two treatments.
Methods
Nineteen patients who received treatment for PCT or TTM after severe TBI between March 2018 and April 2022 were retrospectively enrolled. Medical records were reviewed, including general information, neurologic status, treatment courses, survival rate, and complications. Patients were divided into two groups according to the treatment modalities (PCT vs. TTM), and comparison analyses were conducted.
Results
The survival rate in the TTM group was 33.3% (3/9), which was higher than that in the PCT group (1/10, 10%). However, this difference was not significant (p = 0.213). In terms of complications, there were no statistically significant differences in hemodynamic instability, cardiovascular disability, hepatic dysfunction, renal dysfunction, pneumonia, urinary tract infection, hyperkalemia, hypokalemia, coagulopathy, or hyperglycemia. Commonly observed complications included hypokalemia in the TTM group (100% in the TTM group vs 70% in the PCT group; p = 0.073) and hyperkalemia in the PCT group (50% in the PCT group vs 11.1% in the TTM group; p = 0.069).
Conclusion
Severe TBI patients treated with TTM has non-significantly lower mortality than them with PCT (66.7% vs. 90%); however, complications of hypokalemia can be frequently observed (100%). Further study was necessary to evaluate the efficacy and safety of TTM.
INTRODUCTION
In patients with severe traumatic brain injury (TBI), elevated intracranial pressure (ICP) after primary damage is known to have a significant influence on subsequent outcome1). Therefore, several treatment options are considered for such patients, such as craniectomy with or without hematoma removal, cerebrospinal fluid drainage, hyperosmolar therapy, sedatives, hyperventilation, etc.2). Despite maximum medical and surgical treatment, a large portion of severe TBI patients have poor prognosis. In clinical settings, pentothal coma therapy (PCT) or targeted temperature management (TTM) can be considered.
While two options are regarded as a last-tier non-surgical therapy in severe TBI patients, the previous studies failed to identify the safety and efficacy of the treatments. Therefore, these treatments were regarded as an optional (not-essential) treatment in refractory elevated ICP situations and the comparison between two options were rarely reported1,3).
Here, we reported our experience on two treatments in severe TBI patients and tried to establish a more appropriate treatment by comparing side effects and survival rates between the two treatments.
MATERIALS AND METHODS
Patient selection criteria
This was a retrospective single-center study of patients who received treatment for PCT or TTM between March 2018 and April 2022 at our center. A total of 84 patients underwent PCT or TTM, of which 22 were treated for TBI. Of these, 19 patients were included in the study, except for three who received both treatments concurrently (Figs. 1, 2).
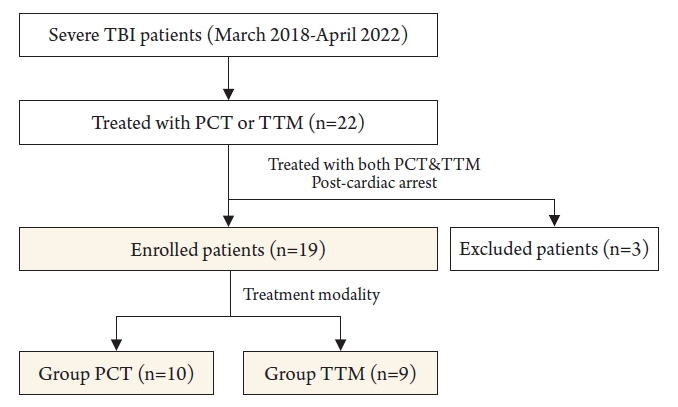
Enrollment flow diagram. The criteria for inclusion and exclusion for patients with TBI are shown.
PCT: Pentothal coma therapy, TTM: Targeted temperature management, TBI: Traumatic brain injury.
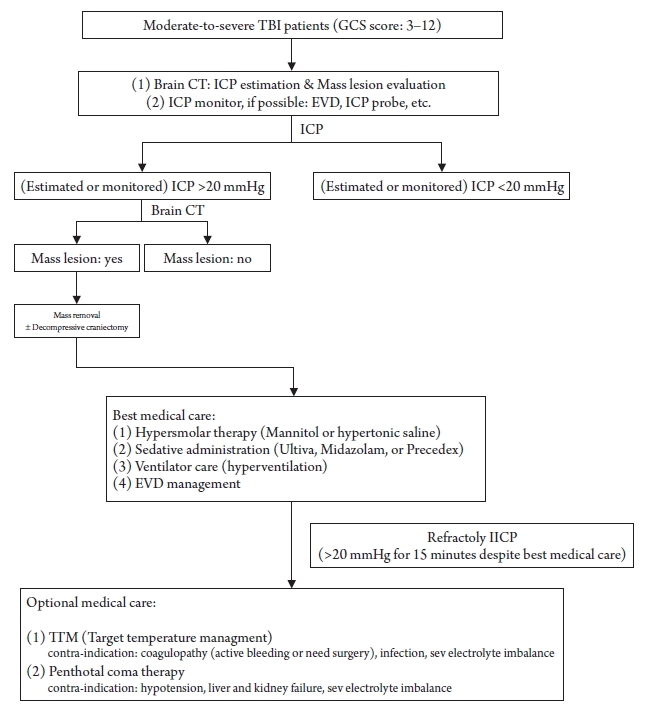
Protocol for the treatment of moderate-to-severe brain injury.
TBI: Traumatic brain injury, GCS: Glasgow coma scale, CT: Computed tomography, ICP: Intracranial pressure, EVD: External ventricular drainage, IICP: Increased intracranial pressure..
Medical records were collected, including age, sex, diagnosis, underlying disease, initial mental status, Glasgow Coma Scale (GCS) score, motor grade, pupillary reflex, and application time. For evaluating prognosis, total hospital stays (day) and mortalities (at 2 weeks, 3 months, and 6 months from the end of treatment) were reviewed. To evaluate side effects, parameters of hemodynamic instability, cardiovascular disability, hepatic dysfunction, renal dysfunction, pneumonia, urinary tract infection, hyperkalemia, hypokalemia, coagulopathy, and hyperglycemia were investigated. Patients were divided into two groups according to the treatment modalities (PCT vs. TTM), and comparative analyses were conducted.
Statistical analyses
Continuous variables were analyzed as mean and standard deviation, and categorical variables were analyzed as numbers and percentages. For the comparison of PCT and TTM, a chi-square test was performed for categorical variables, and an independent t-test was performed for continuous variables. The likelihood ratio was used when cells with an expected frequency less than 5 exceeded 20%. Statistical significance was set to be when the p value was 0.05 or less. IBM SPSS statistics 25ver. was used.
RESULTS
The detailed baseline data are shown in table 1. The mean age of the patient was 68 years, and the mean GCS score was 6. Of these, 11 (57.9%) were male and 8 (42.1%) were female. Subdural hemorrhage (SDH) accounted for the highest rate of diagnosis (47.4 %), and hypertension was the most common underlying disease (47.4%). The overall survival rate was 21.1%, and the rate of treatment termination due to side effects was the highest (84.2%). Of these, 10 patients underwent PCT, and 9 patients underwent TTM.
In table 2, we can see the results of comparison analyses between two groups. No significances were observed between the groups except parameters of ‘treatment days (p=0.004)’ and ‘pupillary reflex (p=0.033). In terms of outcomes, survival rate of TTM group (3/9, 33.3%) is higher than that of PCT group (1/10, 10%), which was not statistically significant (p=0.0213).
In table 3, a comparison of the side effects between the two groups is presented. There were no statistically significant differences in parameters of hemodynamic instability, cardiovascular disability, hepatic dysfunction, renal dysfunction, pneumonia, urinary tract infection, hyperkalemia, hypokalemia, coagulopathy, or hyperglycemia. However, there was a tendency of differences between hyperkalemia and hypokalemia. Hyperkalemia is much frequently observed in PCT group (50% vs. 11.1%), whereas hypokalemia is highly notified in TTM group (70% vs. 100%).
DISCUSSION
Severe TBI patients treated with TTM has non-significantly lower mortality than them with PCT (66.7% vs. 90%); however, complications of hypokalemia can be frequently observed (100%). Further study was necessary to evaluate the efficacy and safety of TTM.
Several studies have been investigated PCT. In 1985, Ward et al. found no significant difference between the standard treatment and PCT on the Glasgow Outcome Scale. However, 40% of patients with TBI in whom ICP control failed despite maximum standard treatment survived at discharge, 68% of which showed good functional outcomes after 1 year4). According to the Brain Trauma Foundation 4th TBI guideline, PCT is recommended for refractory elevated ICP without improvement, despite maximum standard treatment. However, in this case, hemodynamic instability should be carefully adjusted2).
Other studies have shown that PCT causes serious side effects such as hepatic and renal dysfunction, systemic hypotension, immunosuppressive hypokalemia, and rebound hyperkalemia5). RCT in 1985 by Ward et al. showed hypotension was observed in 54% patients with PCT, which was higher than that in the control group (7%, p < 0.001)6).
TTM has also been reported in several studies. TTM has been used as the standard treatment for neuroprotection after cardiac arrest7). Owing to this neuroprotective effect, several studies have been conducted on the treatment of TBI via TTM.
A 2018 meta-analysis showed a decrease in mortality risk of patients with TBI due to the cooling method and slow rewarming8). However, the 2018 study in the Prophylactic Hypothermia Trial to Lessen Traumatic Brain Injury (POLAR) randomized clinical trial (RCT) showed no significant difference in functional outcomes between prophylactic hypothermia and normothermia9). One study reported that hypothermia can cause hypokalemia, hypovolemia, cardiovascular disease, coagulopathy, infection, hyperglycemia, hepatic dysfunction, etc10). Another study reported that there were no significant differences between induced hypothermia and normothermia, despite early induction11). In contrast, another study showed that long-term hypothermia treatment significantly increases the survival rate and functional outcomes in patients with severe TBI, and complications did not show statistical significance12).
Studies on the effects of PCT and TTM have been conducted several times, but studies comparing the side effects of the two treatments are rare. In this study, the differences in the individual side effects between the two groups were not statistically significant (Table 3). However, hyperkalemia tended to be higher in PCT (50% vs. 11.1%, p=0.069), and hypokalemia tended to be higher in TTM (100% vs. 70%, p=0.073). Therefore, it is necessary to monitor the electrolyte imbalance in each treatment.
The survival rate tended to be higher in the TTM group(3 out of 9, 33.3%) than PCT group (1 out of 10, 10%; p=0.213), but it did not show statistical significance (p=0.213; Table 2). However, there was a statistically significant difference in the length of hospitalization and duration of treatment between the two groups (Table 2). It could be interpreted that the duration of treatment of TTM was longer than that of PCT to achieve the same treatment effect. Further studies with larger number of patients will be needed to clarify this tendency.
This study has several limitations. First, this was a retrospective study conducted at a single center; therefore, treatment for patients was not randomly assigned. Second, the sample sizes of the two groups were relatively small. Third, since our center has only 1 ICP monitor, not-all the patient received ICP monitoring, so we were unable to describe the ICP values that were important in determining treatment effects. Fourth, the treatment methods for PCT and TTM were not standardized.
CONCLUSION
Severe TBI patients treated with TTM has non-significantly lower mortality than them with PCT (66.7% vs. 90%); however, complications of hypokalemia can be frequently observed (100%). Further study was necessary to evaluate the efficacy and safety of TTM.
Notes
Conflict of interest
There is no conflict of interest to disclose


