 |
 |
- Search
| J Neurointensive Care > Volume 5(2); 2022 > Article |
|
Abstract
Methods
This was a retrospective, observational study of patient admitted to the neurosurgical intensive care unit (ICU) from January 2013 to December 2019. The subjects were classified into two groups: the non-obese group (body mass index [BMI] < 25 kg/m2) and the overweighted or obese group (BMI ≥ 25 kg/m2). The primary endpoint was in-hospital mortality.
Results
A total of 527 patients were included in this study. The mean BMI was 23.7 ± 3.6 kg/m2. Of all neurosurgical patients, 157 patients were overweighted or obese. There were no significant differences in in-hospital mortality, 28-day mortality, and ICU mortality between the two groups (all p > 0.05). BMI on ICU admission was similar between survivors and non-survivors at discharge (p = 0.596). In the multivariable analysis, Acute Physiology and Chronic Health Evaluation (APACHE) II score on ICU admission, invasive intracranial pressure (ICP) monitoring, and use of more than one hyperosmolar agent were identified to be significantly associated with in-hospital mortality. However, BMI on ICU admission, and serum albumin level were not associated with in-hospital mortality. The obesity demonstrated a borderline significance relationship with the probability of in-hospital mortality (p=0.073).
Conclusion
In this study, BMI on ICU admission, and serum albumin level demonstrated a lack of significant association with in-hospital mortality. Clinical factors including APHCHE II score, ICP monitoring, and hyperosmolar therapy were identified to be associated with prognosis in neurocritically ill patients. Eventually, the impact of the obesity paradox on these patients remains unclear.
Obesity is a public health problem and is generally known to be associated with increased morbidity and mortality due to associated complications1,2). Obesity can increase the risk of many chronic diseases including coronary artery disease, atrial fibrillation, congestive heart failure, diabetes mellitus, and stroke1,3). Therefore, obesity is hypothesized as one of the main factors that lead to the deterioration of health. However, in hospitalized patients, obesity may have the opposite effect compared with the general population. The obesity paradox was found in patients with heart failure and coronary heart disease4). Obesity is associated with cardiovascular disease even in the absence of other risk factors; however, after the onset of cardiovascular disease, the relationship between higher body mass index (BMI) and the clinical prognosis does not demonstrate linearity4). Interestingly, overweighted or obese patients had more favorable outcomes than normal or underweight patients with cardiovascular disease4).
The obesity paradox has also been reported in some neurocritically ill patients1,25-7). Obesity is associated with favorable outcomes in stroke subtypes other than subarachnoid hemorrhages, such as intracerebral hemorrhage1,2,5) and ischemic stroke2,6,7). However, there are limited well-designed clinical studies that prove the exact relationship between BMI and clinical outcomes in neurocritically ill patients. In this study, we aimed to evaluate whether the obesity paradox exists in neurocritically ill patients similar to the case of patients with cardiovascular disease. In addition, we evaluated whether BMI on ICU admission is associated with in-hospital mortality of neurocritically ill patients.
This was a retrospective, single-center, observational study of patients who were admitted to the Samsung Medical Center, Seoul, Republic of Korea, neurosurgical intensive care unit (ICU) from January 2013 to December 2019. This study was approved by the Samsung Medical Center Institutional Review Board (IRB) (IRB no. SMC 2020-09-082). The requirement of informed consent was waived by the IRB due to the study’s retrospective nature. We included neurosurgical patients who were hospitalized in the ICU during the study period. We defined neurocritically ill patients as neurosurgical patients who were hospitalized in the ICU for more than 7 days due to postoperative management or critical care following brain tumor, subarachnoid hemorrhage, cerebral vascular surgery, intracerebral hemorrhage, cerebral infarction, traumatic brain injury or infection of the central nervous system. We excluded patients aged below 18 years, those who did not have the value of BMI or a brain injury, or those who had insufficient medical records or a ‘do not resuscitation’ order.
In this study, the baseline characteristics such as comorbidities, behavioral risk factors, ICU management, and laboratory data were collected retrospectively using Clinical Data Warehouse. Our center constructed a “Clinical Data Warehouse Darwin-C” designed for the investigators to search and retrieve de-identified medical records from electronic archives. The subjects were classified into two groups: the non-obese group (BMI < 25 kg/m2) and the overweighted or obese group (BMI ≥ 25 kg/m2)1,8). BMI was obtained on ICU admission. Albumin was defined as a minimal level of serum albumin within 72 h from ICU admission. Acute Physiology and Chronic Health Evaluation (APACHE) II score was calculated with the worst values recorded during the initial 24 h after the ICU admission9,10). If the patient was intubated, the verbal score of the Glasgow Coma Scale was estimated using the eye and motor scores as described previously11). In this study, the primary endpoint was in-hospital mortality.
All data are presented as mean ± standard deviation for continuous variables or frequencies and proportions for categorical variables. Data were compared using Student’s t-test for continuous variables and Chi-square test or Fisher’s exact test for categorical variables. Variables with a p-value less than 0.2 in univariate analyses and clinically relevant variables, including age, sex, BMI, albumin, comorbidities, cause of ICU admission, utilization of organ support modalities, use of invasive intracranial pressure (ICP) monitoring device, hyperosmolar therapy, and APACHE II score, were subjected to stepwise multiple logistic regression analysis to obtain statistically meaningful predictors of in-hospital mortality. All the tests were two-sided and p values of less than 0.05 were considered statistically significant. All the statistical analyses were performed with R Statistical Software version 4.0.2 (R Foundation for Statistical Computing, Vienna, Austria).
A total of 12,743 patients were admitted to the neurosurgical ICU during the study period. Among these neurosurgical patients, 527 neurocritically ill patients were included in the final analysis. The mean BMI was 23.7 ± 3.6 kg/m2. Of all neurocritically ill patients, 157 (29.8%) patients were overweighted or obese. Malignancy (60.2%) and hypertension (44.4%) were the most common comorbidities among the selected patients. Brain tumor (41.4%) and stroke (31.7%) were the most common reasons for ICU admission. There were no significant differences in baseline characteristics between overweighted or obese and non-obese patients except for the prevalence of hypertension and hyperosmolar therapy (Table 1).
There were no significant differences in in-hospital mortality, 28-day mortality, and ICU mortality between the two groups (all p > 0.05). In addition, there were no significant differences in hospital and ICU stay between the groups (both p > 0.05) (Table 2). BMI on ICU admission was similar between the survivors and non-survivors at discharge (p = 0.596) (Fig. 1).
In the multivariable analysis, APACHE II score on ICU admission (adjusted odds ratio [OR]: 1.09, 95% confidence interval [CI]: (1.04–1.14), invasive ICP monitoring (adjusted OR: 0.39, 95% CI: 0.20–0.74), and use of more than one hyperosmolar agent (adjusted OR: 2.24, 95% CI: 1.1–4.23) were identified to be significantly associated with in-hospital mortality (Table 3). In this study, BMI on ICU admission, and serum albumin level were not associated with in-hospital mortality. The relationship between BMI and probability of in-hospital mortality was shown in Fig. 2. However, the obesity demonstrated a borderline significance relationship with the probability of in-hospital mortality (adjusted OR: 0.32, 95% CI: 0.09–1.08, p=0.073).
In this study, we investigated the existence of the obesity paradox in neurocritically ill patients. About 30% of patients were either overweighted or obese. There was no significant difference in BMI between the survivors and non-survivors. In addition, there were no significant differences in in-hospital mortality, 28-day mortality, ICU mortality, and length of stay in ICU and hospital between the overweighted or obese and non-obese patients. In the multivariable analysis, APACHE II score on ICU admission, invasive ICP monitoring, and use of more than one hyperosmolar agent were identified to be significantly associated with in-hospital mortality. However, BMI on ICU admission, and serum albumin level demonstrated a lack of association with in-hospital mortality. In this study, the obesity demonstrated a borderline significance relationship with the probability of in-hospital mortality.
Obesity is a well-known risk factor for an increased incidence of heart failure and coronary heart disease4). However, the patients with class I obesity and these heart diseases present a more favorable outcome compared with normal or underweight subjects. Therefore, this phenomenon is termed the “obesity paradox”. Obesity is strongly associated with the occurrence of ischemic heart disease even in the absence of other risk factors. However, the relationship between higher BMI and clinical outcomes is not linear in patients with ischemic heart disease4). The obesity paradox has been reported in patients with trauma as well 12). In addition, previous studies have reported the presence of the obesity paradox in patients admitted to the ICU for sepsis, severe sepsis, and septic shock13-15).
BMI on ICU admission has been reported to be associated with the nutritional status of the patient on ICU admission16). Nutrition is an important aspect of the management of patients hospitalized in the ICU17-19). Especially, malnutrition is associated with prolonged hospitalization and duration of mechanical ventilation, increased prevalence of infection, and mortality in critically ill patients18,20,21). In addition, malnutrition is also associated with poor clinical outcomes in neurocritically ill patients22-24). Loss of skeletal muscle mass could develop after ICU admission25). In the early stage, loss of muscle mass and malnutrition have been reported to be associated with clinical outcomes in neurocritically ill patients26-28). Malnutrition has been evaluated based on various parameters such as BMI, serum albumin, and skeletal muscle mass18). However, BMI and serum albumin are not considered useful parameters to accurately assess the nutritional status of critically ill patients17,18). Whereas, measurement of skeletal muscle mass is known as a more accurate parameter in representing the nutritional status. The change in skeletal muscle mass may reflect the clinical prognosis compared to other nutritional measures in critically ill patients18). In neurocritically ill patients, knowledge about early nutritional status and its change are important for neurological prognosis 22-24). Also, rapidly progressing sarcopenia has been reported to be associated with poor prognosis26-28), but this change was not evaluated in the present study.
In this study, clinical factors such as APACHE II score, ICP monitoring, and hyperosmolar therapy were identified to be associated with prognosis in neurocritically ill patients. To date, it remains unclear whether the obesity paradox can be observed in neurocritically ill patients2,29-31). Generally, the causes of early mortality in neurocritically ill patients are primary brain injury, and refractory intracranial hypertension or herniation due to severe brain edema32). Therefore, it is possible to determine the patient’s prognosis based on the primary and secondary brain injuries rather than nutritional status in the early stage. Henceforth, neurocritically ill patients who survived for more than a week were included in this study. However, obesity assessed by BMI on ICU admission did not appear to reflect the nutritional status and prognosis of these patients.
This study has several limitations. First, this was a retrospective review of medical records using data extracted from a Clinical Data Warehouse. The nonrandomized data might lead to selection bias. Second, lean body mass and loss of muscle mass were not evaluated. Therefore, it might be difficult to access the precise nutritional status and its change of neurocritically ill patients. Third, it might be difficult to find statistically meaningful variables because the proportion of non-survivor compared with a survivor was very low in this study. Finally, the distribution of causes of ICU admission in the postoperative group was different from that of the general neurosurgical ICU group, and the proportion of patients with brain tumors was particularly high.
In this study, BMI on ICU admission, and serum albumin level demonstrated a lack of significant association with in-hospital mortality. Clinical factors including APHCHE II score, ICP monitoring, and hyperosmolar therapy were identified to be associated with prognosis in neurocritically ill patients. Eventually, the impact of the obesity paradox on the survival of neurocritically ill patients remains unclear, and further studies are needed to evaluate the relationship between obesity and clinical outcomes in neurocdritically ill patients.
Acknowledgements
We would like to thank Suk Kyung Choo, the nursing director of the neurosurgical intensive care unit, for providing excellent advice and engaging in fruitful discussions. We would also like to thank all nurses of the neurosurgery intensive care unit at the Samsung Medical Center.
Fig. 1.
Body mass index of survivors and non-survivors. There was no significant difference between the two groups (p = 0.596).
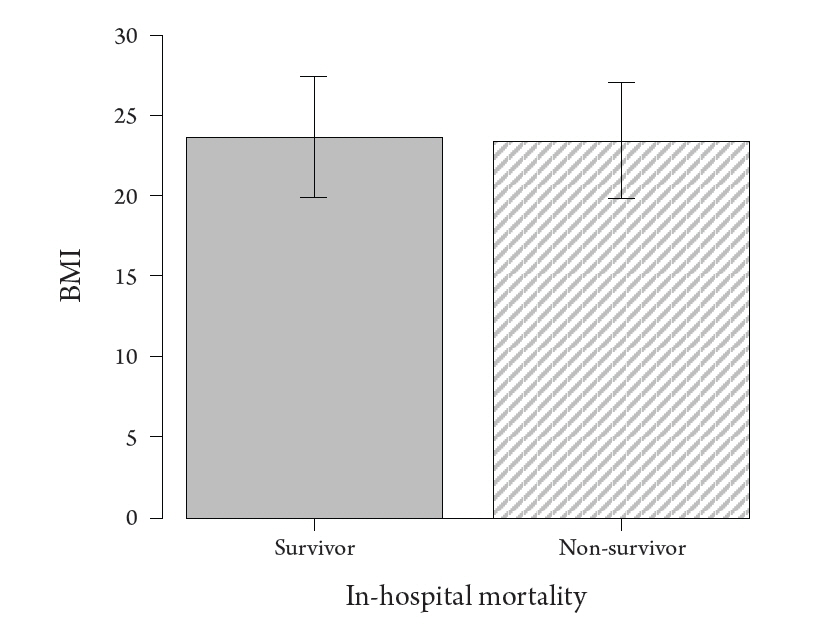
Fig. 2.
The probability of in-hospital mortality according to body mass index within the multivariate model.

Table 1.
Baseline characteristics according to obesity
Table 2.
Clinical outcomes according to obesity
Table 3.
Multivariable logistic regression of clinically relevant variables associated with in-hospital mortality.
| Adjusted odds ratio (95% CI) * | p-value | |
|---|---|---|
| BMI (kg/m2) | 1.06 (0.91-1.23) | 0.454 |
| Obesity | 0.32 (0.09-1.08) | 0.073 |
| Albumin (g/dL) | 0.64 (0.32-1.28) | 0.204 |
| APACHE II score on ICU admission | 1.09 (1.04-1.14) | <0.001 |
| Invasive ICP monitoring | 0.39 (0.20-0.74) | 0.004 |
| Use of more than one hyperosmolar agent | 2.24 (1.18-4.23) | 0.013 |
* Adjusted for BMI, albumin, age, sex, comorbidities, cause of ICU admission, utilization of organ support modalities, use of invasive ICP monitoring device, hyperosmolar therapy, and APACHE II score.
CI: Confidence interval, BMI: Body mass index, APACHE: Acute Physiology and Chronic Health Evaluation, ICP: Intracranial pressure.
REFERENCES
1. Dangayach NS, Grewal HS, De Marchis GM, Sefcik RK, Bruce R, Chhatlani A, et al. Does the obesity paradox predict functional outcome in intracerebral hemorrhage? J Neurosurg 2018;129:1125–1129.


2. Rautalin I, Kaprio J, Korja M. Obesity paradox in subarachnoid hemorrhage: a systematic review. Neurosurg Rev 2020;43:1555–1563.



3. Zalesin KC, Franklin BA, Miller WM, Peterson ED, McCullough PA. Impact of obesity on cardiovascular disease. Med Clin North Am 2011;95:919–937.


4. Carbone S, Canada JM, Billingsley HE, Siddiqui MS, Elagizi A, Lavie CJ. Obesity paradox in cardiovascular disease: where do we stand? Vasc Health Risk Manag 2019;15:89–100.


5. Kim BJ, Lee SH, Ryu WS, Kim CK, Lee J, Yoon BW. Paradoxical longevity in obese patients with intracerebral hemorrhage. Neurology 2011;76:567–573.


6. Kim Y, Kim CK, Jung S, Yoon BW, Lee SH. Obesity-stroke paradox and initial neurological severity. J Neurol Neurosurg Psychiatry 2015;86:743–747.


7. Wohlfahrt P, Lopez-Jimenez F, Krajcoviechova A, Jozifova M, Mayer O, Vanek J, et al. The obesity paradox and survivors of ischemic stroke. J Stroke Cerebrovasc Dis 2015;24:1443–1450.


8. Patel JJ, Rosenthal MD, Miller KR, Codner P, Kiraly L, Martindale RG. The Critical Care Obesity Paradox and Implications for Nutrition Support. Curr Gastroenterol Rep 2016;18:45.



9. Capuzzo M, Valpondi V, Sgarbi A, Bortolazzi S, Pavoni V, Gilli G, et al. Validation of severity scoring systems SAPS II and APACHE II in a single-center population. Intensive Care Med 2000;26:1779–1785.



10. Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med 1985;13:818–829.


11. Meredith W, Rutledge R, Fakhry SM, Emery S, Kromhout-Schiro S. The conundrum of the Glasgow Coma Scale in intubated patients: a linear regression prediction of the Glasgow verbal score from the Glasgow eye and motor scores. J Trauma 1998;44:839–844; discussion 844-835.

12. Dvorak JE, Lester ELW, Maluso PJ, Tatebe L, Schlanser V, Kaminsky M, et al. The Obesity Paradox in the Trauma Patient: Normal May not Be Better. World J Surg 2020;44:1817–1823.




13. Arabi YM, Dara SI, Tamim HM, Rishu AH, Bouchama A, Khedr MK, et al. Clinical characteristics, sepsis interventions and outcomes in the obese patients with septic shock: an international multicenter cohort study. Crit Care 2013;17:R72.



14. Jagan N, Morrow LE, Walters RW, Plambeck RW, Wallen TJ, Patel TM, et al. Sepsis and the obesity paradox: size matters in more than one way. Crit Care Med 2020;48:e776–e782.


15. Karvetski C, Templin M, Herlihy JD, Taylor B. Do-Not-Resuscitate status explains the obesity paradox in patients with severe sepsis, in d24. critical care: the other half of the icu - update in management of non-pulmonary critical care. 2017;a7152–a7152.
16. Borel A-L, Schwebel C, Planquette B, Vésin A, Garrouste-Orgeas M, Adrie C, et al. Initiation of nutritional support is delayed in critically ill obese patients: a multicenter cohort study. The American Journal of Clinical Nutrition 2014;100:859–866.


17. Higgins PA, Daly BJ, Lipson AR, Guo SE. Assessing nutritional status in chronically critically ill adult patients. Am J Crit Care 2006;15:166–177.




18. Moisey LL, Mourtzakis M, Cotton BA, Premji T, Heyland DK, Wade CE, et al. Skeletal muscle predicts ventilator-free days, ICU-free days, and mortality in elderly ICU patients. Crit Care 2013;17:R206.



19. Puthucheary ZA, Rawal J, McPhail M, Connolly B, Ratnayake G, Chan P, et al. Acute skeletal muscle wasting in critical illness. Jama 2013;310:1591–1600.


20. Dvir D, Cohen J, Singer P. Computerized energy balance and complications in critically ill patients: an observational study. Clin Nutr 2006;25:37–44.


21. Villet S, Chiolero RL, Bollmann MD, Revelly JP, Cayeux RNM, Delarue J, et al. Negative impact of hypocaloric feeding and energy balance on clinical outcome in ICU patients. Clin Nutr 2005;24:502–509.


22. Sabbouh T, Torbey MT. Malnutrition in Stroke Patients: Risk Factors, Assessment, and Management. Neurocritical care 2018;29:374–384.




23. Wang X, Dong Y, Han X, Qi XQ, Huang CG, Hou LJ. Nutritional support for patients sustaining traumatic brain injury: a systematic review and meta-analysis of prospective studies. PLoS One 2013;8:e58838.



24. Yoo SH, Kim JS, Kwon SU, Yun SC, Koh JY, Kang DW. Undernutrition as a predictor of poor clinical outcomes in acute ischemic stroke patients. Arch Neurol 2008;65:39–43.


25. Santilli V, Bernetti A, Mangone M, Paoloni M. Clinical definition of sarcopenia. Clin Cases Miner Bone Metab 2014;11:177–180.



26. Leitner J, Pelster S, Schopf V, Berghoff AS, Woitek R, Asenbaum U, et al. High correlation of temporal muscle thickness with lumbar skeletal muscle cross-sectional area in patients with brain metastases. PLoS One 2018;13:e0207849.



27. Ranganathan K, Terjimanian M, Lisiecki J, Rinkinen J, Mukkamala A, Brownley C, et al. Temporalis muscle morphomics: the psoas of the craniofacial skeleton. J Surg Res 2014;186:246–252.


28. Swartz JE, Pothen AJ, Wegner I, Smid EJ, Swart KM, de Bree R, et al. Feasibility of using head and neck CT imaging to assess skeletal muscle mass in head and neck cancer patients. Oral Oncol 2016;62:28–33.


29. Abhyankar S, Leishear K, Callaghan FM, Demner-Fushman D, McDonald CJ. Lower short- and long-term mortality associated with overweight and obesity in a large cohort study of adult intensive care unit patients. Crit Care 2012;16:R235.



30. Hogue CW Jr., Stearns JD, Colantuoni E, Robinson KA, Stierer T, Mitter N, et al. The impact of obesity on outcomes after critical illness: a meta-analysis. Intensive Care Med 2009;35:1152–1170.



- TOOLS
-
METRICS

-
- 0 Crossref
- 1,507 View
- 44 Download
- Related articles in JNIC
-
Association of Hyponatremia and Clinical Prognosis in Neuro Critically Ill Patients2021 April;4(1)
Prognostic Value of Early Hyperglycemia in Neurocritically Ill Patients2020 April;3(1)





