Neurotrauma Code: Proposal for the Implementation of Strategies in Areas of Difficult Care for a Time-dependent Condition.
Article information
An adequate configuration of health systems for the care of time-dependent pathologies is essential to ensure a favorable out for patients. Various pathologies where care is time-dependent, have protocols such as stroke code, trauma code, cardiac arrest code among others1). These processes are in place and most are activated in anticipation of a complex condition that is life-threatening, requires multiple health disciplines, and is time-sensitive.
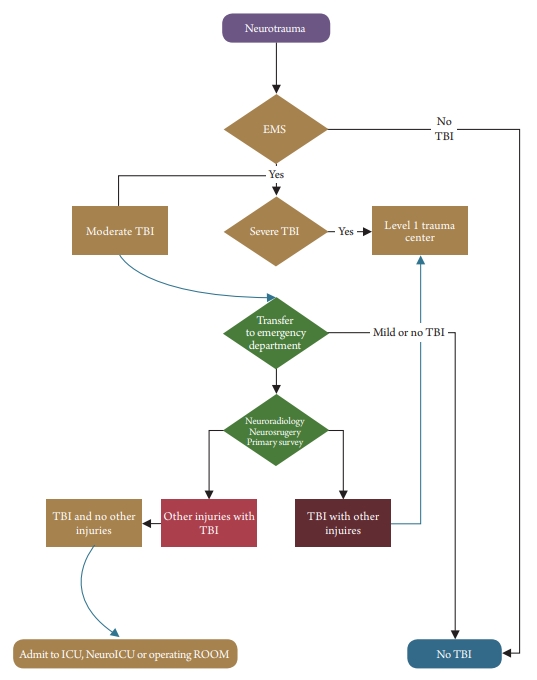
Neurotrauma as pathology is a common reason for the utility of health services and intensive care units2). This affects the population of different ages and with high mortality. In low-income countries where the availability of resources is limited, we believe that there should be the categorization of neurotrauma. This process will allow the referral of only patients requiring neurosurgical and neurointensive care. For this, we propose the designation of Neurotrauma Code, which would be activated only focus on moderate head trauma (The one described by Glasgow coma scale 9-13, post-resuscitation).
The process starts in the field with moderate injury and activation is initiated once transport begins. The emergency department will respond with proper triage, assessment, and investigations. Once neurotrauma is considered the main diagnosis, the neurosurgery and radiology department is activated. Primary and secondary surveys need to be done This might require emergency room physicians to be trained in this process. This will be required as trauma surgeons are usually assigned to a level 1 trauma center, where they are dealing with all types of traumas. The patient will be either send to general critical care ICU, neuro floor unit or transfer to level 1 trauma center based upon the kind of injury. We can see this process helping all sorts of acute care health care institutions. Neurotrauma code can also be useful for level 1 trauma centers. These centers are mostly overwhelmed with extensive polytrauma patients, gunshot wounds, falls injuries, motor-vehicle injuries, and assault victims. Moderate neurotrauma might get a somewhat delayed response and activation of neurotrauma code will help to stop the acute injury process early before it progresses to a severe or irreversible stage.
In conclusion, neurotrauma code (Fig. 1) has a unique need in the bigger scope of trauma and neurocritical care fields. Health care organizations without level 1 trauma centers will benefit from the process to take care of their patients. Level 1 trauma centers with extremely busy services will be able to early recognize moderate head injury patients and place them in the proper treatment pathway.
Notes
Conflict of interest
No potential conflict of interest relevant to this article was reported.