Characteristics of Traumatic Brain Injury Patients in Korean Military Hospitals During Non-War Years
Article information
Abstract
Objective
Because of the specialty of the military medical system, there might be different characteristics of patients with traumatic brain injury (TBI) comparing to the patients in university hospitals. However, the characteristics of the soldiers’ TBI has never been reported. Therefore, we tried to identify the different characteristics of TBI patients in military hospitals by comparing them of other hospitals.
Methods
We extracted the data of TBI patients from the databank of the Korean Multicenter TBI study. Patients, who were diagnosed with TBI and admitted to the ten institutions (including two military hospitals) between January 2016 and December 2018, were retrospectively enrolled. They are divided into ‘Military’ and ‘Other’ groups according to the admitted hospitals, and statistical comparisons were conducted on gathered information.
Results
Among 4601 enrolled patients, 133 patients were from two military hospitals and 4468 patients belong to the eight university hospitals. Military patients show significant younger age and male predominance. In general, they have fewer past histories and different trauma mechanisms - more sports-related and lesser traffic accident-related. They usually show higher initial Glasgow coma scale scores and better favorable outcomes - lower incidence of neurologic deterioration in mild TBIs and better modified Rankin Scale scores in moderate to severe TBIs.
Conclusions
Military hospitals usually take care of small numbers of patients who are young males with mild TBIs. Because of the different characteristics of group members and traumatic severity, the patients usually show favorable outcomes. Therefore, the optimized medical system is mandatory.
INTRODUCTION
In 1953, the Armed Forces Medical Command of Republic of Korea (ROK) was established. It provided medical service and welfare for the military service personnel6). Up to date, it offers several military hospitals distributed near corps and is able to handle the situation of potential mass casualties after wartime. Because of the huge gap between the numbers of the patients in wartime and those in non-wartime, military hospitals usually utilize the different medical systems according to the situations3,4,11). During the non-war years (a confrontation with the North), military medical service usually takes care of small numbers of the patients; therefore, a few military hospitals are concentrated and equipped with the medical resources to treat the severe traumatic brain injury (TBI) patients. However, the characteristics of the military personnel’s TBI in ROK during the non-war years has never been reported; and the majority of the literatures on military TBI are limited to the wartime situation such as combat injuries1,7,9).
By the merest chance, two military hospitals (AFCH, Armed Forces Capital Hospital; and AFYH, Armed Forces Yangju Hospital) participated in the Korean multi-centered TBI (KMTBI) study for identifying the clinical features and analyzing risk factors for young TBI patients. They constructed a large databank which includes patients diagnosed with TBI for 3 consecutive years (2016~2018) in participants’ hospitals. By using these data, we could identify the different characteristics of the military personnel’s TBI comparing to those of the general populations. It might be helpful to understand the characteristics of military TBIs and to optimize the military medical systems in non-wartime situations.
MATERIALS AND METHODS
Patients and data acquisition
The data were extracted from the registered data bank system from the KMTBI study. Ten institutions (eight university hospitals and two military hospitals) are participated in the KMTBI study. The patients, who were admitted to the hospitals and diagnosed with definitive TBI from January 2016 to December 2018, were retrospectively enrolled. Patients, who were aged under 15 or who had poor medical records, were excluded. In this study, the data were registered online and were freely accessible to the research team of the institutions. The extracted data contained age, sex, past medical histories, mechanism of trauma, diagnosis, neurologic status including Glasgow coma scale (GCS) scores, treatment modality, and outcomes. The outcome was measured by the modified Rankin Scale scores on discharging date in mild TBI and at six-month in moderate to severe TBIs. In addition, the neurological deterioration was defined when the GCS score decrement is larger than 2 points. The previous study was approved by the Institutional Review Board of the Human Research Center of each institution. The requirement for obtaining informed consent was omitted because it is a retrospective design.
In the current study, the patients were divided into “Military Hospital” group and “Other Hospital” group according to the institution that the patients are admitted to. In addition, patients were classified as mild (13-15) and moderate/severe TBIs (3-12) according to their GCS scores.
Statistical analysis
Baseline characteristics of military hospital groups were examined. Furthermore, comparison analyses between the groups were conducted by two steps; “mild” and “moderate/severe” TBIs according to the GCS scores. Continuous values were presented as mean and standard deviation, and they were compared by using independent t-test. Discontinuous variable data were presented as numbers and percentages, and they were compared by using Chi-square analysis. Statistical analyses were conducted using a standard software (version 23.0, SPSS, IBM, Chicago, IL, USA), and the significance was considered if p < 0.05.
RESULTS
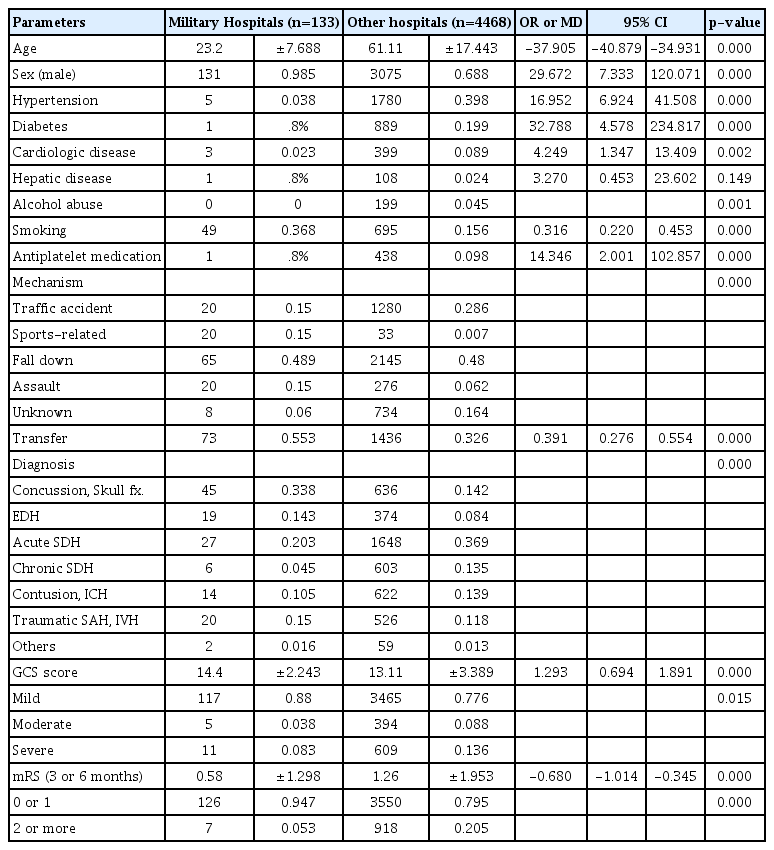
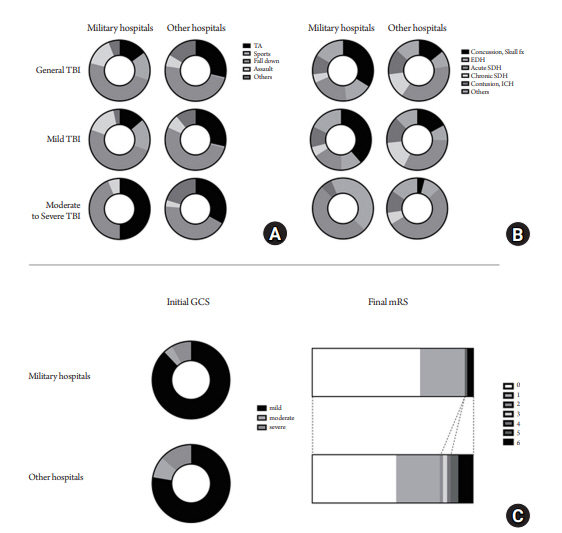
Table 1 demonstrates the comparison of general demographics between military and other hospital groups. Total 133 patients (107 from AFCH and 26 from AFYH) were identified as the military personnel, and they were young and had male predominance with significances. They have less past medical histories including hypertension, diabetes, cardiologic disease, alcohol abuse, and antiplatelet agent medications. In terms of TBI mechanism, they significantly have more frequent association with sports and less association with traffic accidents. More than a half of the military personnel were transferred from other hospitals (55.3%). Regarding diagnosis, concussion and epidural hematoma were more frequent in military group, whereas acute and chronic subdural hematoma were highly occurred in other hospital groups. In military group, most of the patients had mild TBI (88.0%) with better initial GCS scores (14.40±2.24). Consequently, the outcome of modified Rankin Scale (mRS) was favorable in military group.
Table 2 shows the results of comparison between the groups in ‘mild TBI’. The GCS score is significantly higher in military group. Non-specific symptoms such as headache, dizziness, nausea and vomiting, and loss of consciousness are more frequently occurred in military group, and motor weakness is often observed in other hospital groups. Most of the military patients received conservative treatment without surgical interventions, and the outcome (incidence of neurological deterioration, decrement in GCS score >2) was more favorable. The mRS score is slightly higher in military personnel, and it is not significant.
Table 3 presents the results of comparison between the groups in ‘moderate to severe TBIs’. Initial neurologic status according to the GCS score, mental status, symptoms, and signs have no significant differences between the groups. However, the military personnel significantly show favorable outcomes in 3 or 6-months mRS scores.
The TBI mechanism (A), initial diagnosis (B), initial GCS score and 6-month mRS score (C) are illustrated in Fig. 1.
DISCUSSION
Herein, we tried to figure out the different clinical features of military personnel’s TBI comparing to the general populations. In general, the military personnel are significantly young and healthy (lower rate of having past medical histories) and show high male predominance. They showed better prognosis including lesser neurologic deterioration in mild TBIs (p=0.004) and lower mRS scores at 3 or 6 months in moderate to severe TBIs (p=0.001). From military medical perspective, military personnel’s TBI should be optimized because of their lesser TBI events and better prognosis.
The TBI patients from military hospitals have never been reported due to the following reasons. First, the incidence of head trauma in the military corps is relatively low due to the limited social activities of the military personnel and their efforts for reducing a non-combat injury. Second, majority of military hospitals’ members is consisted of short-term working military officers (3 to 5 years), and they rarely investigate or report the literatures. Third, due to the situation of prolonged confrontation against the North, the military remains tense and is separated from the society in terms of location as well as a scholastic exchange. Also, the process of the military medical investigation is quite complicated.
Characteristics of military TBIs during the non-war years
The result of the current study would be a good reference for the military doctors working in the military hospitals. In order to identify the clinical characteristics of the military TBI patients, the optimized military medical system can be equipped during this non-war years in ROK. They can place the medical resources in the right place with the most efficient ways. Specifically, the most of the patients in military group are young male soldiers, and they show the clinical differences: lesser past medical diseases, higher incidence of sports-related trauma, lower incidence of traffic accidents, and lesser frequent diagnosis of chronic subdural hematoma12,13). We conclude that the military hospital usually cares mild TBI patients, that the most of them is young male soldiers. Only 10% of the military patients had severe TBI, and others had favorable outcomes which means non-severe TBI (Table 1).
From the ‘mild TBI’ comparison (Table 2), we can draw a conclusion that the clinical manifestation, clinical courses, and outcomes of military mild TBI patients are related to ‘young male’ patients. The patients significantly complain bitterly of non-specific symptoms: headache, dizziness, nausea and vomiting, and loss of consciousness. A larger number of young patients might be related to the sensitive detection of increased intracranial pressure, and the symptoms can be frequently observed among the young age group. On contrary, ‘motor weakness’ is significantly highly observed among other hospital groups: it might be related to the chronic subdural hemorrhage which frequently occurred in elderly patients10). Therefore, the treatment such as burr-hole trephination is more frequently conducted in other hospital groups. In terms of outcome, we can find that no military patients were deteriorated, which means that the military personnel in mild TBI have rarely been worsened to moderate or severe TBIs.
In moderate to severe TBIs (Table 3), the favorable clinical courses and outcome in military personnel are identified. The initial neurologic status, including GCS scores, level of consciousness, and neurological symptom and signs, have no differences between the groups. Treatment modality does not vary among the groups, neither. However, the mRS score in military group is approximately 1 point higher than that in other hospital groups. Because more than a half of the military patients who had no symptoms or had mild symptoms (mRS 0 to 1) were treated, physicians should actively treat the patients.
Clinical implication of the study
We identify the low incidence of TBI in military personnel and small numbers of ‘severe’ patients which requires the human as well as medical resources for treating. In non-wartime years, the military hospitals in ROK divided their works and specialties for better efficacy. If we have TBI patients (especially, severe), they initially visit the nearest military hospital and are transferred to the superior hospitals. Consequently, AFCH carries on providing the medical service as the supremacy hospital. In addition, AFYH is located on front lines and usually prepare for the potential combat injuries. Maybe this systematic difference leads to the higher transfer rates of military hospitals (55.3%). Instead, the medical command operates an all-time helicopter emergency transporting systems in order to assess and manage the patients better2). The fastest transporting system may enable the better clinical outcomes. According to our results, two hospitals greatly manage the military TBI patients, and the outcomes are favorable.
Limitations
The present study has several limitations. First, the data were extracted from the databank system of KMTBI, and they did not include radiological images. Therefore, known prognostic factors observed in brain computed tomography (CT), such as poor Marshall or Rotterdam CT scores, were omitted5,8). Second, the data were registered from each different hospital’s reviewers, and there might be an inter-observer bias.
CONCLUSIONS
Military hospitals usually take care of young male soldiers with mild TBIs. Because of the different characteristics of group members and traumatic severity, the patients usually survive and show favorable outcomes. Therefore, the optimized treatment should be mandatory.
Notes
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Acknowledgements
The clinical data was obtained from the database of Korean Multi-centered Traumatic Brain Injury 2019 study (KMTBI-2019).
The authors appreciate to the 10 principal investigators of each institution: Seong-Jong Lee, Sang Hoon Yoon, Ki Seong Eom, Kyung-Jae Park, Sung-Kon Ha, Jin-gyu Choi, Kwang Wook Jo, Suk Hyung Kang, Jongyeon Kim, and Jong Hyun Kim.