Current Prophylactic Hypothermia for Intracranial Hypertension after Traumatic Brain Injury
Article information
Abstract
Hypothermia performed in patients with traumatic brain injury (TBI) reduces cerebral metabolism and cerebral blood flow, subsequently decreasing intracranial pressure (ICP). There have been many disagreements about the effectiveness of prophylactic hypothermia in its clinical application. Until now, hypothermia has been used without standardized treatment guidelines and performed by each medical provider's personal judgment. Recently, a large-scale randomized controlled trial regarding hypothermia was conducted, and it concluded that the early use of therapeutic hypothermia in the staged management of ICP elevation is not beneficial. Therefore, it is our latest knowledge that it is difficult to derive a standardized treatment protocol for prophylactic hypothermia in TBI patients, and also, it is not advantageous to the patient.
INTRODUCTION
After a report on the effect of hypothermia on minimizing brain damage following cardiac arrest, many hypothermia studies have been conducted on patients with traumatic brain injury (TBI)1-3). Among them, there were studies that hypothermia in TBI patients lowers intracranial pressure (ICP) caused by cerebral edema and improves the patient's outcome4). On the other hand, in a recent multicenter randomized controlled trial (RCT) study in adults, the authors concluded that the effect of hypothermia treatment could not be confirmed5). There have been disagreements regarding the effectiveness of hypothermia for patients with TBI. A large number of medical providers are in effort to set a standard treatment guideline for hypothermia after TBI patients to use hypothermia as a complementary treatment option of controlling ICP. Since then, large-scale studies have been conducted on the application of hypothermia to patients with TBI in various centers under different conditions. Therefore, we would like to examine the possibility of deriving a standard treatment guideline by analyzing the clinical applications and treatment outcome of hypothermia for patients with TBI, recently published through several large-scale studies.
PATHOPHYSIOLOGY
When the body temperature decreases, the brain's metabolism decreases by 6-10% per degree, and the energy demand decreases6). As the cell membrane is stabilized, the indiscriminate influx of sodium and calcium ions and consequent cerebral edema decreases7). In addition, hypothermia suppresses apoptosis, reduces the influx of polymorphonuclear leukocytes into the brain tissue and secretion of cytokines, thereby reducing the inflammatory response. As a result, it shows a neuroprotective effect and a decrease in ICP caused by ischemia or TBI8,9).
CLINICAL APPLICATIONS OF HYPOTHERMIA
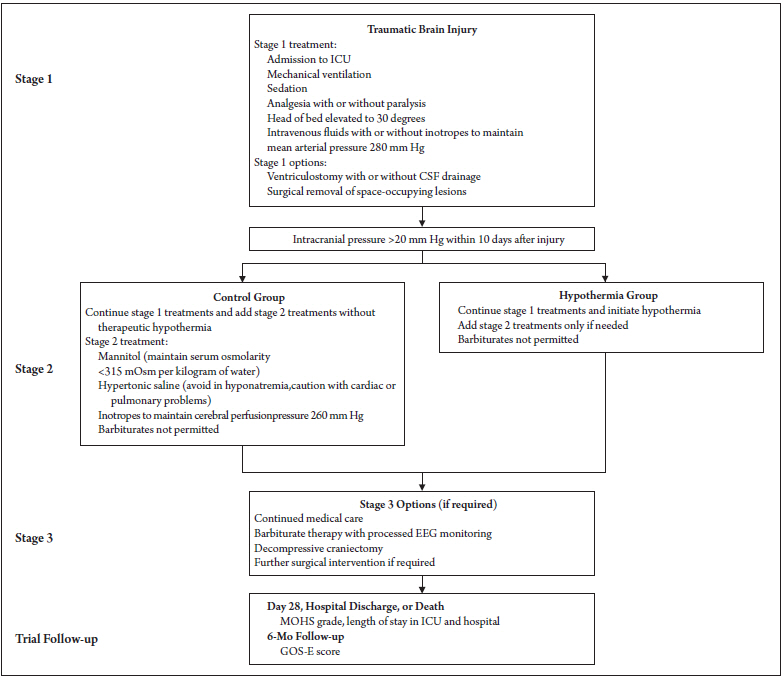
Hypothermia was induced for TBI patients who were unresponsive to stage 1 treatments (defined as mechanical ventilation, sedation, head of bed to 30°, analgesia, cerebral perfusion pressure optimization, +/- ventriculostomy, or +/- surgical removal of space-occupying lesions) and who were ICP of >20 mmHg for at least 5 minutes10,11). A bolus of intravenous, refrigerated 0.9% sodium chloride (20 to 30 ml per kilogram of body weight) was administered and after that maintained with each site's usual cooling technique. Patients randomized into the hypothermia group received therapeutic temperature modulation (TTM) with an initial target of 35°C 12), but the temperature was lowered incrementally down to as low as 32 °C until ICP was below 20 mmHg. Hypertonic solutions were then administered only if hypothermia was ineffective. Patients in the control group received hypertonic solutions once stage-1 therapies had failed to bring the ICP to ≤ 20 mmHg. Once hypothermia started, it was maintained for at least 48 h and then re-warmed at a rate of 0.25°C per hour if ICPs were under control. The primary outcome was scored using the Extended Glasgow Outcome Scale (GOS-E) at 6 months (Fig. 1)11).
TREATMENT EFFECT OF HYPOTHERMIA
According to the previously published meta-analysis regarding the role of hypothermia in patients with TBI, hypothermia showed significant improvement on survival rate and functional recovery rate13,14). Contrary to the previous knowledge, a recently conducted multicenter RCT study concluded that hypothermia did not lead to any positive outcomes than conventional treatment11,15,16). While prophylactic hypothermia after TBI has been extensively studied in the “National Acute Brain Injury Study: Hypothermia” (NABISH)15) trials and “Prophylactic Hypothermia Trial to Lessen Traumatic Brain Injury” (POLAR) RCT with little success, the specific use of “late-rescue” hypothermia to treat intracranial hypertension after TBI has acquired less attention16). EuroTherm3235, another open-label RCT study, compared use versus non-use of hypothermia prior to administering hypertonic solutions as a part of a staged treatment of intracranial hypertension after TBI11). In contrast to expectations, hypothermia did not show a superior effect compared to conventional treatment in large-scale studies. One of the possible explanations for no change would be the timing of rewarming coinciding with the point at which cerebral edema worsens17). Other feasible reasons include TBI's mechanism being different from that of brain injury caused by cardiac arrest and medical provider's ineptness in controlling the patient's fluid volume and blood pressure17).
The trial was initially designed to enroll 600 patients. However, it terminated early after recording and randomizing 387 subjects due to undesirable outcomes in the hypothermia group. The adjusted common odds ratio for the GOS-E score was 1.53 (95% confidence interval, 1.02 to 2.30; P=0.04), indicating that the hypothermia group had a more unsatisfactory outcome than in the control group. A favorable outcome (GOS-E score of 5 to 8, indicating moderate disability or good recovery) was yielded in 26% of the patients in the hypothermia group compared to 37% in the control group (p=0.03)11). This trial addressed convincing evidence that application of hypothermia to 32-35 °C likely has more risks than benefits for treatment of intracranial hypertension in TBI10).
However, many centers still perform hypothermia when the following conditions arise during the treatment of traumatic brain injury patients, and these conditions have not been studied in Eurotherm3235 trials10).
a) Use only after hypertonic solutions have failed,
b) For more severe ICP elevations (> 25–30 mmHg), or
c) Only after barbiturate coma has failed.
The efficacy of hypothermia in these clinical situations remains unclear, especially with patients who have severe, refractory elevated ICP. Many centers still continue to utilize TTM management to 33 °C for patients with ICP > 25 mmHg who have failed hypertonic solutions in order to reduce the use of barbiturate-induced coma. However, there is no evidence refuting nor supporting this treatment.
CONCLUSION
The early use of therapeutic hypothermia in the staged management of ICP elevation is not beneficial10). There is also growing evidence that prophylactic hypothermia does not improve patients' outcomes and does not have a significant effect on intracranial hypertension. As stated in the earlier NABISH trials, it is our latest knowledge that it is difficult to derive a standard treatment protocol for prophylactic hypothermia in TBI patients, and also it is not beneficial to the patient.
Notes
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Acknowledgements
The authors thank Dr. Jennifer Bai for her help in manuscript translation.