Superior Mesenteric Infarction During Management of Patient with Cerebral Infarction
Article information
Abstract
Acute mesenteric ischemia may be defined as a sudden interruption of the blood supply to a segment of the small intestine. The overall incidence is low but mortality is high(50-80%). These cases show a very rare case that the patient with intracerebral hemorrhage was combined AMI. The patient is finally undergoing emergency surgery and is being treated. We report that multiple complications should be considered during treatment of cerebral hemorrhage.
INTRODUCTION
Acute mesenteric ischemia (AMI) is caused by insufficient blood supply to a part of the small intestine. This causes ischemia, cellular damage, intestinal necrosis, and sometimes leads to death1). The primary etiology of AMI was found to mesenteric arterial embolism (50%), mesenteric arterial thrombosis (15–25%), or mesenteric venous thrombosis (5–15%)2,3). Half of AMI are related to cardiac dysrhythmias such as atrial fibrillation, myocardial dysfunction, poor ejection fraction, or cardiac valves dysfunction. Early diagnosis is possible with CT4). Appropriate diagnosis and treatment increases survival rates5,6).
CASE REPORT
A 82-year-old female visited emergency center(Korea University Anam Hospital) with sudden onset of left hemiparesis after her awakening. She has been managed for arterial fibrillation and stable angina, and mitral valve disease, and anti-coagulation treatment warfarin was done since the day before visit. Initial GCS score was 14(E3-V5-M6), and motor grade of left side was grade III. Facial asymmetry was observed, and mild dysarthria was comorbid. Initial NIHSS score was 21, and modified Rankin scale was 5.
Initial bran CT scan revealed ICH on right parietal lobe, and peri-regional low attenuation was observed. Presentation on CT was not usual ICH pattern, so CT angiography for evaluation for ruled out acute infarction with hemorrhagic transformation was followed. CT angiography revealed embolic infarction of left MCA territory (Fig. 1). Due to ICH, intravenous t-PA was absolutely contraindicated, so general conservative management was done. Anticoagulant was stopped due to ICH.

Initial CT scan revealed ICH on right parietal lobe, and CT angiography revealed acute embolic infarction on right MCA territory.
During admission to ICU, she presented consistant arterial fibrillation. Cardiology consultation was done, and rate and blood pressure was controlled with calcium-channel blocker. Although CCB administration, her rate and arterial fibrillation was not controlled. So, digitalization with digoxin was started at hospital day 3. Despite all general care, patients underwent neurologic deterioration. Initially she presented nearly alert mentality, but about hospital day 3, she presented confused mentality. Hemiparesis of left side was worsened to grade I. Follow-up brain imaging was performed, but no significant change was observed. Until then, we presumed neurologic deterioration was due to cerebral infarction, so generalized heart management and ICP control was done.
From hospital day 5, she presented high fever. Due to her mentality, no other complaint was observed. Routine fever study was performed, and empirical antibiotics was started ampicillin-sulbactam) for HAP. But fever was not subsided, and further evaluation was needed. At hospital day 8, abdominal CT was performed for fever study.
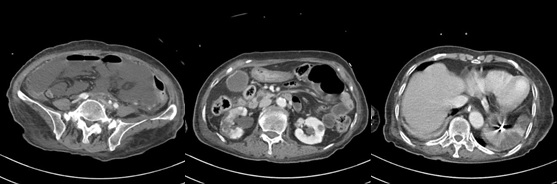
Abdominal CT revealed extensive small bowel infarction. Infarction was extended to mid-jejunal loop to terminal ileum with large amount of complicated fluid collection and peritonitis. CT revealed multifocal low-attenuating lesions on spleen and right kidney, suggesting splenic and renal infarction (Fig. 2). The day after diagnosis of small bowel infarction, emergent surgery was performed by CRS doctor. Small bowel was resected, and end jejunostomy was performed. Small intestine was resected about 182 centimeters long, and remnant small bowel was only upper jejunum for 80 centimeters long. Pathology report confirmed multiple thrombi in mesenteric blood vessel. For management of small bowel infarction due to embolic event, anticoagulation was re-started with LMWH, and 3 days after surgery, warfarin was restarted. Despite anticoagulation treatment, parietal ICH on right side was not worsened, and patient underwent post-operative management in CRS department.
DISCUSSION
In our case, patient cannot present abdominal symptoms due to her mentality. Furthermore, around the time she presented fever, her chest X-ray revealed diffuse haziness, so empirically selected antibiotics was administrated. If emergent abdominal evaluation was performed, we could seize the chance of early diagnosis.
Retrospectively reviewed, the patient presented with a cerebral infarction that had a stable angina history due to arterial fibrillation and was thought to be due to an embolic event. After hospitalization, arterial fibrillation continued, and histories were consistent with known etiology of the AMI7). It is not wrong to think of brain etiology as primary for the situation where the patient's consciousness is deteriorated during hospitalization due to cerebral infarction. It is also important to note that worsening on chest X-rays was observed and that many patients with cerebral infarction show similar progression and therefore do not require additional testing in most cases. Of course, fasting state was maintained for a long time after hospitalization and the patient was not aware of the abdominal symptoms due to decreased consciousness, but more meticulous observations and examinations should be performed.
CONCLUSION
We presented a rare case of AMI during admission due to cerebral infarction. AMI is rare but devastating condition so called true surgical emergency. It is relatively rare, but in patients with arterial fibrillation, meticulous clinical assessment should be needed.
Notes
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Acknowledgements
None.