|
 |
- Search
| J Neurointensive Care > Volume 4(1); 2021 > Article |
|
Abstract
Objective
To investigate the impact of hyponatremia severity on in-hospital mortality of neurocritically ill patients.
Methods
This was a retrospective, observational study of patients who were admitted at a tertiary university hospital, Seoul, Republic of Korea, neurosurgical intensive care unit (ICU) from January 2013 to December 2019. We included neurocritically ill patients whose serum sodium concentrations were obtained during the ICU admission. The primary endpoint was in-hospital mortality.
Results
A total of 903 patients were included in the final analysis. Hyponatremia was detected in 359 (39.8%) patients. There was no significant difference in in-hospital mortality between the no hyponatremia group and the hyponatremia group (8.8% vs. 9.7%, p = 0.724). However, the length of ICU stay was longer in the hyponatremia group than no hyponatremia group (282.3 ┬▒ 295.9 hr vs. 141.8 ┬▒ 89.3 hr, p < 0.001). In the multivariable analysis, severe hyponatremia (adjusted odds ratio [OR]: 5.41, 95% confidence interval [CI]: 1.23 ŌĆō 20.54), malignancy (adjusted OR: 3.45, 95% CI: 1.29 ŌĆō 9.72), continuous renal replacement therapy (adjusted OR: 6.15, 95% CI: 1.65 ŌĆō 23.38), invasive intracranial pressure monitoring (adjusted OR: 0.39, 95% CI: 0.17 ŌĆō 0.83) and Glasgow Coma Scale on ICU admission (adjusted OR: 0.6, 95% CI: 0.52 ŌĆō 0.69) were significantly associated with in-hospital mortality.
Conclusion
Based on our findings, mild to moderate hyponatremia were not associated with clinical outcomes. However, severe hyponatremia was significantly associated with in-hospital mortality. Therefore, adequate and timely regulation of serum sodium level is important for favorable prognosis and survival of neurocritically ill patients.
Hyponatremia is a common electrolyte abnormality in hospitalized patients6,9,13,17). It could be mild with nausea and vomiting or severe with lethargy, seizures, and loss of consciousness14). In the critically ill, especially neurocritically ill patients, hyponatremia is also a common electrolyte disorder and is associated with clinical prognosis13,14). Hyponatremia may induce neurological complications including cerebral edema, increased intracranial pressure (ICP), seizures, altered mentality, and brain death due to exacerbation of brain edema6). In addition, neurocritically ill patients may be more vulnerable to hyponatremia and may develop clinical symptoms in the absence of severe hyponatremia6,16). Therefore, inadequate or delayed hyponatremia treatment may lead to significant morbidity and mortality13) in neurocritically ill patients. However, the number of studies that have reported the correlation between hyponatremia severity and the clinical outcomes of neurocritically ill patients is limited. In this study, we aimed to evaluate the impact of hyponatremia severity on in-hospital mortality of neurocritically ill patients.
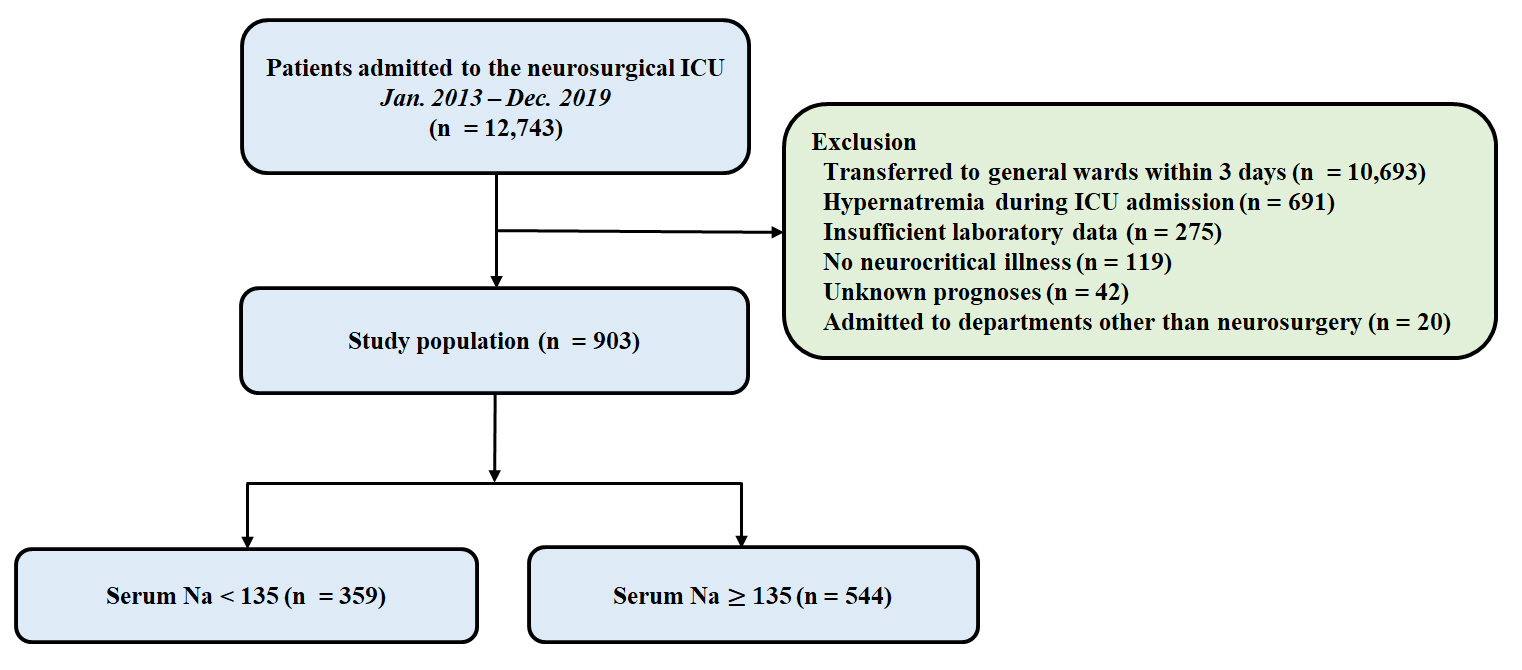
This was a retrospective, single-center, observational study of patients who were admitted at the Samsung Medical Center, Seoul, Republic of Korea, neurosurgical intensive care unit (ICU) from January 2013 to December 2019. This study was approved by the Institutional Review Board (IRB) of Samsung Medical Center (IRB approval number: SMC 2020-09-082). PatientsŌĆÖ records were reviewed and analyzed according to the Declaration of Helsinki. The requirement of informed consent was waived by the IRB due to its retrospective nature. We included neurocritically ill patients and those who were on neurosurgical postoperative management, including brain tumor, subarachnoid hemorrhage, cerebral vascular surgery, intracerebral hemorrhage, cerebral infarction, traumatic brain injury, infection of the central nervous system. In addition, the patients should have been hospitalized in the ICU for more than 3 days or died within 3 days after ICU admission, and their serum sodium concentrations should have been obtained during the ICU admission. We excluded patients whose hypernatremia was above 145 mEq/L during their ICU stay, who had insufficient medical records, who had a ŌĆśdo not resuscitationŌĆÖ order, who were admitted to departments other than neurosurgery, and who were transferred to other hospitals or with unknown prognosis (Fig. 1).
In this study, the baseline characteristics such as comorbidities, behavioral risk factors, ICU management, and laboratory data were collected retrospectively using Clinical Data Warehouse. Our center constructed a ŌĆ£Clinical Data Warehouse Darwin-CŌĆØ designed for investigators to search and retrieve de-identified medical records from electronic archives. The serum sodium levels were obtained at least once every day from all neurosurgical patients. Hyponatremia was defined as serum sodium < 135 mmol/L5). In addition, to help determine the association between the clinical outcomes and severity of hyponatremia, the patients were categorized into four subgroups: no hyponatremia (Ōēź135mEq/L), mild hyponatremia (130 ŌĆō 134mEq/L), moderate hyponatremia (125 ŌĆō 129mEq/L), and severe hypernatremia (<125mEq/L)5). In this study, the primary endpoint was in-hospital mortality.
All data are presented as mean ┬▒ standard deviation for continuous variables or frequencies and proportions for categorical variables. Data were compared using StudentŌĆÖs t-test for continuous variables and Chi-square test or FisherŌĆÖs exact test for categorical variables. A stepwise multiple logistic regression was performed to obtain a statistically meaningful predictor of in-hospital mortality. All tests were two-sided and p values of less than 0.05 were considered statistically significant. All statistical analyses were performed with R Statistical Software version 4.0.2 (R Foundation for Statistical Computing, Vienna, Austria).
A total of 12,743 patients were admitted to the neurosurgical ICU during the study period, among them 903 patients were included in the final analysis. The mean age of all the patients was 44.9 ┬▒ 24.4 years and 54.0% of patients were male. Hyponatremia was detected in 359 (39.8%) patients. Malignancy (66.0%) and hypertension (37.1%) were the most common comorbidities, while brain tumors (52.2%) and intracerebral hemorrhage (12.7%) were the most common reasons for ICU admission (Table 1).
There was no significant difference in in-hospital mortality between the no hyponatremia group and the hyponatremia group (8.8% vs. 9.7%, p = 0.724). However, the length of ICU stay was longer in the hyponatremia group than no hyponatremia group (282.3 ┬▒ 295.9 hr vs. 141.8 ┬▒ 89.3 hr, p<0.001). In addition, there were no significant differences in the clinical outcome according to the hyponatremia severity-based groups except hospital length of stay (p < 0.001) (Table 2).
In the multivariable analysis, severe hyponatremia (adjusted odds ratio [OR]: 5.41, 95% confidence interval [CI]: 1.23 ŌĆō 20.54), malignancy (adjusted OR: 3.45, 95% CI: 1.29 ŌĆō 9.72), continuous renal replacement therapy (adjusted OR: 6.15, 95% CI: 1.65 ŌĆō 23.38), invasive ICP monitoring (adjusted OR: 0.39, 95% CI: 0.17 ŌĆō 0.83) and Glasgow Coma Scale on ICU admission (adjusted OR: 0.6, 95% CI: 0.52 ŌĆō 0.69) were significantly associated with in-hospital mortality (Table 3).
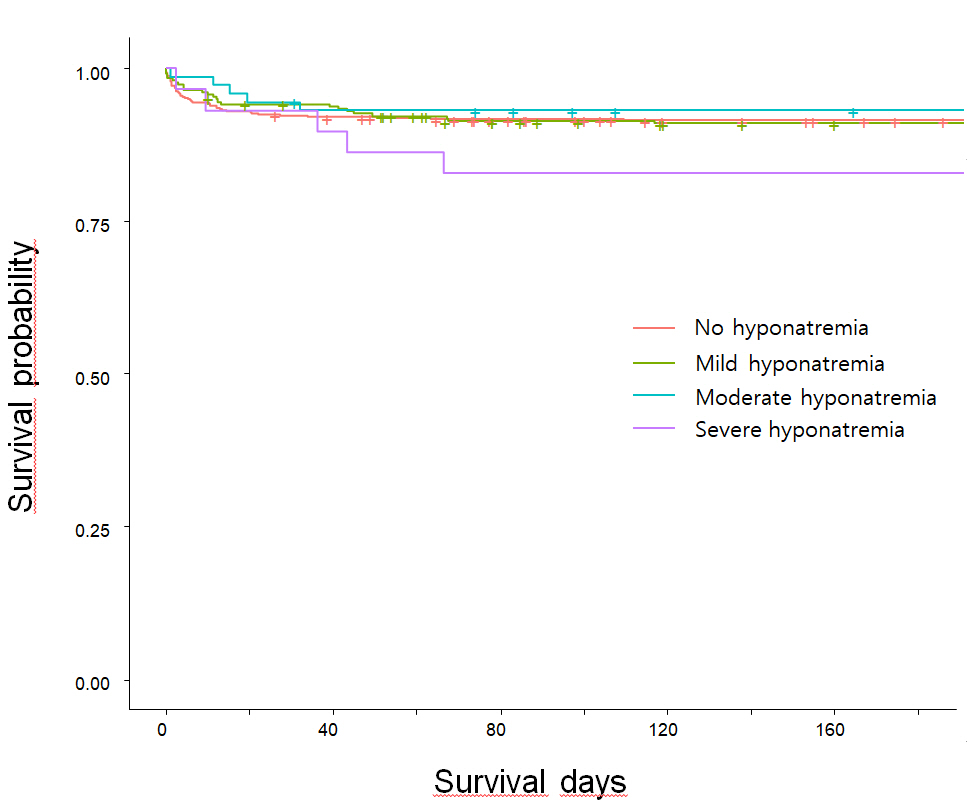
In the survival rate analysis, the patients with severe hyponatremia had the worst survival rate among the overall patients. However, there were no significant differences in the mortality rates of patients according to the severity of hyponatremia (p = 0.430, Fig. 2).
In this study, we investigated the impact of hyponatremia on in-hospital mortality of neurocritically ill patients. Major findings of this study were as follows. First, based on our findings, approximately one-third of the neurocritically ill patients had hyponatremia during their ICU stay. However, there was no significant difference in in-hospital mortality between the no hyponatremia group and the hyponatremia group. There were also no significant differences in the clinical outcome among the hyponatremia severity based. On the other hand, the length of ICU stay was longer in the hyponatremia group than in the no hyponatremia group. Although hyponatremia did not show significant association with clinical outcomes in the univariable analysis, severe hyponatremia showed significant association with mortality in multivariable analysis. In addition, the multivariable analysis revealed that severe hyponatremia, malignancy, continuous renal replacement therapy, invasive ICP monitoring, and Glasgow Coma Scale on ICU admission were significantly associated with in-hospital mortality.
Hyponatremia is the most common electrolyte abnormality in hospitalized patients3) and especially the neurocritically ill patients9); previous studies reported hyponatremia in up to 38 % of critically ill patients and up to 50 % of neurosurgical patients2,7,9,16,19). Although the pathophysiology of hyponatremia in neurocritically ill patients is multifactorial, cerebral salt wasting syndrome and syndrome of inappropriate antidiuretic are the most common causes of hyponatremia in these patients6,9,13). Hyponatremia has been associated with the clinical progress of neurocritically ill patients9,13,15). Acute hyponatremia can cause brain edema and rapid neurological deterioration by increasing the osmotic gradient between the cerebral interstitial tissue and serum9). If prolonged, hyponatremia even in mild cases can lead to increased intracranial pressure, neurological abnormalities, and even death4,9). Some complications, such as hyponatremic seizures, are more prevalent in severe cases of hyponatremia than in benign disease9). For instance, the clinical manifestations of hyponatremia are severe in neurocritically ill patients with intractable intracranial hypertension, severe brain damage, or neurosurgical intervention6,16).
Similar to the previous reports, in this study, hyponatremia was also a common electrolyte abnormality in neurocritically ill patients. However, most hyponatremia cases were mild and only 3% of all patients showed severe hyponatremia. In the present study, severe hyponatremia was a significant predictor of in-hospital mortality, while mild to moderate hyponatremia were not associated with clinical outcomes. However, these findings are inconsistent with previous studies6,16). Even patients with normal sodium level or hyponatremia were excluded from this study if they had a history of hypernatremia during ICU hospitalization. Several studies revealed that hypernatremia was associated with poor clinical outcomes in neurocritically ill patients8,10,11,18). Although hyperosmolar therapy is the standard approach to the treatment of intracranial hypertension in the neurocritically ill patients, it is associated with hypernatremia and hyperosmolar therapy-induced acute kidney injury that can aggravate hypernatremia1,11,18). In addition, hypothalamic dysfunction due to brain injury can contribute to hypernatremia12,18). Therefore, ICU-acquired hypernatremia is a possible complication in severe brain injuries. For this study, it is possible that some patients with severe brain injuries were excluded due to accompanied hypernatremia.
This study has several limitations. First, this was a retrospective review of medical records using data extracted from a Clinical Data Warehouse. The nonrandomized nature of registry data might have resulted in a selection bias. Second, the duration of hyponatremia and correction of serum sodium was not reflected in this study. Third, most hyponatremia cases were mild with only a small percentage of severe hyponatremia cases. Finally, the distribution of neurosurgical diseases was different from that in the general neurosurgical ICU, and the proportion of patients with brain tumors was particularly high.
Based on our study findings mild to moderate hyponatremia were not associated with clinical outcomes in neurocritically ill patients. However, severe hyponatremia was significantly associated with in-hospital mortality. Therefore, adequate and timely regulation of serum sodium level is important for favorable prognosis and survival of neurocritically ill patients.
Acknowledgements
We would like to thank Hye Jung Kim, the nursing director of the neurosurgical intensive care unit, for providing excellent advice and engaging in fruitful discussions. We would also like to thank all nurses of the neurosurgery intensive care unit at Samsung Medical Center.
Table┬Ā1.
Baseline characteristics
| Variable | Normal (n = 544) | Hyponatremia (n = 359) | p value |
|---|---|---|---|
| Patient demographics | |||
| ŌĆāAge (year) | 43.4 ┬▒ 24.1 | 47.2 ┬▒ 24.7 | 0.021 |
| ŌĆāSex, male | 276 (50.7) | 212 (59.1) | 0.017 |
| Comorbidities | |||
| ŌĆāMalignancy | 332 (61.0) | 264 (73.5) | <0.001 |
| ŌĆāHypertension | 147 (27.0) | 112 (31.2) | 0.200 |
| ŌĆāDiabetes mellitus | 44 (8.1) | 41 (11.4) | 0.118 |
| ŌĆāChronic kidney disease | 19 (3.5) | 31 (8.6) | 0.002 |
| ŌĆāCardiovascular disease | 19 (3.5) | 13 (3.6) | 0.999 |
| ŌĆāChronic liver disease | 13 (2.4) | 12 (3.3) | 0.518 |
| Behavioral risk factors | |||
| ŌĆāCurrent alcohol consumption | 100 (18.4) | 68 (18.9) | 0.901 |
| ŌĆāCurrent smoking | 55 (10.1) | 38 (10.6) | 0.906 |
| Cause of ICU admission | 0.017 | ||
| ŌĆāBrain tumor | 276 (50.7) | 195 (54.3) | |
| ŌĆāIntracerebral hemorrhage | 69 (12.7) | 46 (12.8) | |
| ŌĆāVascular surgery | 70 (12.9) | 34 (9.5) | |
| ŌĆāTraumatic brain injury | 54 (9.9) | 35 (9.7) | |
| ŌĆāSubarachnoid hemorrhage | 52 (9.6) | 34 (9.5) | |
| ŌĆāCentral nervous system infection | 8 (1.5) | 14 (3.9) | |
| ŌĆāCerebral infarction | 15 (2.8) | 1 (0.3) | |
| APACHE II score on ICU admission | 5.0 ┬▒ 5.0 | 5.9 ┬▒ 5.5 | 0.006 |
| Glasgow Coma Scale on ICU admission | 13.1 ┬▒ 2.4 | 13.0 ┬▒ 2.3 | 0.696 |
| ICU management | |||
| ŌĆāMechanical ventilation | 182 (33.5) | 162 (45.1) | 0.001 |
| ŌĆāContinuous renal replacement therapy | 10 (1.8) | 12 (3.3) | 0.225 |
| ŌĆāInvasive ICP monitoring | 206 (37.9) | 177 (49.3) | 0.001 |
| ŌĆāUse of mannitol* | 268 (49.3) | 140 (39.0) | 0.003 |
| ŌĆāUse of glycerin* | 141 (25.9) | 96 (26.7) | 0.843 |
| ŌĆāUse of vasopressors | 36 (6.6) | 26 (7.2) | 0.819 |
Table┬Ā2.
Clinical outcome according to the severity of hyponatremia
Table┬Ā3.
Multivariable analysis of in-hospital mortality according to the severity of hyponatremia
| Variable | Adjusted odds ratio (95% CI)* | p value |
|---|---|---|
| Hyponatremia | ||
| ŌĆāNo hyponatremia | 1 | Reference |
| ŌĆāMild hyponatremia | 0.92 (0.45 ŌĆō 1.85) | 0.818 |
| ŌĆāModerate hyponatremia | 0.54 (0.12 ŌĆō 1.87) | 0.368 |
| ŌĆāSevere hyponatremia | 5.41 (1.23 ŌĆō 20.54) | 0.017 |
| Malignancy | 3.45 (1.29 ŌĆō 9.72) | 0.016 |
| Continuous renal replacement therapy | 6.15 (1.65 ŌĆō 23.38) | 0.007 |
| ICP monitoring | 0.39 (0.17 ŌĆō 0.83) | 0.019 |
| Glasgow Coma Scale on ICU admission | 0.60 (0.52 ŌĆō 0.69) | < 0.001 |
REFERENCES
1. Aiyagari V, Deibert E, Diringer MN. Hypernatremia in the neurologic intensive care unit: how high is too high? J Crit Care 2006;21:163ŌĆō172.


2. Bennani SL, Abouqal R, Zeggwagh AA, Madani N, Abidi K, Zekraoui A, et al. [Incidence, causes and prognostic factors of hyponatremia in intensive care]. Rev Med Interne 2003;24:224ŌĆō229.


3. Boscoe A, Paramore C, Verbalis JG. Cost of illness of hyponatremia in the United States. Cost Eff Resour Alloc 2006;4:10.



4. DeVita MV, Gardenswartz MH, Konecky A, Zabetakis PM. Incidence and etiology of hyponatremia in an intensive care unit. Clin Nephrol 1990;34:163ŌĆō166.

5. Fogarty J, Loughrey C. Hyponatraemia in Hospitalised Adults: a Guide for the Junior Doctor. Ulster Med J 2017;86:84ŌĆō89.


7. Hoorn EJ, Lindemans J, Zietse R. Development of severe hyponatraemia in hospitalized patients: treatment-related risk factors and inadequate management. Nephrol Dial Transplant 2006;21:70ŌĆō76.


8. Hu B, Han Q, Mengke N, He K, Zhang Y, Nie Z, et al. Prognostic value of ICU-acquired hypernatremia in patients with neurological dysfunction. Medicine (Baltimore) 2016;95:e3840.



9. Kirkman MA, Albert AF, Ibrahim A, Doberenz D. Hyponatremia and brain injury: historical and contemporary perspectives. Neurocrit Care 2013;18:406ŌĆō416.


10. Kolmodin L, Sekhon MS, Henderson WR, Turgeon AF, Griesdale DE. Hypernatremia in patients with severe traumatic brain injury: a systematic review. Ann Intensive Care 2013;3:35.



11. Li M, Hu YH, Chen G. Hypernatremia severity and the risk of death after traumatic brain injury. Injury 2013;44:1213ŌĆō1218.


12. Maggiore U, Picetti E, Antonucci E, Parenti E, Regolisti G, Mergoni M, et al. The relation between the incidence of hypernatremia and mortality in patients with severe traumatic brain injury. Crit Care 2009;13:R110.



13. Manzanares W, Aramendi I, Langlois PL, Biestro A. Hyponatremia in the neurocritical care patient: An approach based on current evidence. Med Intensiva 2015;39:234ŌĆō243.


14. Padhi R, Panda BN, Jagati S, Patra SC. Hyponatremia in critically ill patients. Indian J Crit Care Med 2014;18:83ŌĆō87.



15. Qureshi AI, Suri MF, Sung GY, Straw RN, Yahia AM, Saad M, et al. Prognostic significance of hypernatremia and hyponatremia among patients with aneurysmal subarachnoid hemorrhage. Neurosurgery 2002;50:749ŌĆō755; discussion 755-746.


16. Sherlock M, O'Sullivan E, Agha A, Behan LA, Rawluk D, Brennan P, et al. The incidence and pathophysiology of hyponatraemia after subarachnoid haemorrhage. Clin Endocrinol (Oxf) 2006;64:250ŌĆō254.


17. Vachharajani TJ, Zaman F, Abreo KD. Hyponatremia in critically ill patients. J Intensive Care Med 2003;18:3ŌĆō8.


- TOOLS
-
METRICS

-
- 0 Crossref
- 3,400 View
- 104 Download
- Related articles in JNIC
-
Association of Obesity With Clinical Outcomes in Neurocritically Ill Patients2022 October;5(2)
Prognostic Value of Early Hyperglycemia in Neurocritically Ill Patients2020 April;3(1)